Expression of estrogen receptor, progesterone receptor and KI 67 in epithelial ovarian tumors and their histopathological correlation
Abstract
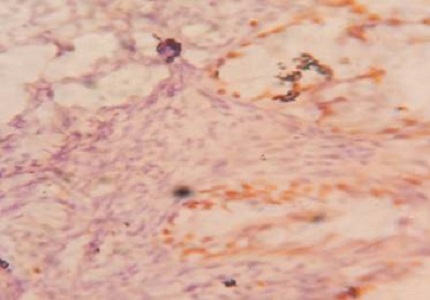
Introduction: Expression of ER, PR and Ki 67 in epithelial ovarian tumors and their histopathological correlation analyzed by immunohistochemistry.
Methods: This study was conducted on 60 ovarian specimens received in Department of Pathology, Gandhi Medical College, Bhopal for ovarian tumors from 1st January 2012 -31st august 2016.
Results: The expression of ER was more in malignant tumor 21/26 than borderline 5/9 and benign tumors 5/25. The PR expression was more in benign tumors 14/25 than malignant 13/26 and borderline 2/9 tumors. The Ki67 expression was more in malignant tumors 22/26 than borderline 7/9 and benign 1/25 tumors.
Conclusion: In our study ER and Ki-67 positivity was maximally seen in malignant cases. This shows that ER was enhanced in ovarian carcinoma and Ki67 was proliferative marker. PR expression was maximally seen in benign tumors. This showed protective role of PR marker in ovarian carcinoma.
Downloads
References
Benson RC, Diagnosis and treatment, current obstetrics gynaecol 1976, 1:236.
Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer J Clin. 2009 Jul-Aug;59(4):225-49. doi: https://doi.org/10.3322/caac.20006. Epub 2009 May 27.
Mylonas I, Jeschke U, Shabani N, Kuhn C, Kriegel S, Kupka MS, Friese K. Normal and malignant human endometrium express immunohistochemically estrogen receptor alpha (ER-alpha), estrogen receptor beta (ER-beta) and progesterone receptor (PR). Anticancer Res. 2005 May-Jun;25(3A):1679-86.
Pertschuk LP, Beddee AM, Gorelic LS, Shain SA immune cytochemicalassay of estrogen receptor in endometroidcarcinoma with monoclonal antibodies Cancer 1986;57:1000-1004.
IsolaJ, Kallioniem OP, Korte JM, Walstrom T, Anie R et all 1990 steroid receptors and Ki 67 reactivity in ovarian cancer in normal ovary, correlation with DNA flow cytometry biochemical receptor assay and patient survival. 1992 Sep; 141(3): 699–706.
G scambia, G Ferrandina, G D Agostino, A Fagotti, M DI Stefano, F Fanfani, F G Serri and S Mancuso. Oestrogen and progesterone receptors in ovarian cancer. Endocrine-Related cancer 1998,5;293-301.
Hall PA, Levison DA. Review: assessment of cell proliferation in histological material. J Clin Pathol. 1990 Mar;43(3):184-92.
Yang, X.-Y., Xi, M.-R., Yang, K.-X. & Yu, H. Prognostic value of estrogen receptor and progesterone receptor status in Chinese young ovarian carcinoma patients. Gynecol Oncol 2009 April 113(1), 99–104.
Nodin, B. et al. Increased androgen receptor expression in serous carcinoma of the ovary is associated with an improved survival. J Ovarian Res 2010 June; 3(14),1757-2215.
Liu P, Sun YL, Du J, Hou XS, Meng H. CD105/Ki67 coexpression correlates with tumor progression and poor prognosis in epithelial ovarian cancer. Int J Gynecol Cancer. 2012 May;22(4):586-92. doi: http://dx.doi.org/10.1097/IGC.0b013e31823c36b8.
T. T. Sreeja and others, ‘A Study on Expression of P53 in Surface Epithelial Ovarian Tumours’, Indian Journal of Mednodent and Allied Sciences, 2016 July; 3(7): 150-158.
Naik PS, Deshmukh S, Khandeparkar SG, Joshi A, Babanagare S, Potdar J, Risbud NS. Epithelial ovarian tumors: Clinicopathological correlation and immunohistochemical study. J Midlife Health. 2015 Oct-Dec;6(4):178-83. doi: https://dx.doi.org/10.4103%2F0976-7800.172349.
Sylvia MT, Kumar S, Dasari P. The expression of immunohistochemical markers estrogen receptor, progesterone receptor, Her-2-neu, p53 and Ki-67 in epithelial ovarian tumors and its correlation with clinicopathologic variables. Indian J Pathol Microbiol. 2012 Jan-Mar;55(1):33-7. doi: http://www.ijpmonline.org/text.asp?2012/55/1/33/94852.
R. Jha and S. Karki, ‘Histological Pattern of Ovarian Tumors and Their Age Distribution’, Nepal Medical College Journal: NMCJ, (2008), 10(2 ) 81–85.
SantoshKumar Mondal and others, ‘Histologic Pattern, Bilaterality and Clinical Evaluation of 957 Ovarian Neoplasms: A 10-Year Study in a Tertiary Hospital of Eastern India’, Journal of Cancer Research and Therapeutics, (2011)Jan, 7(4); 433-37.
Prat J. Ovarian carcinomas, including secondary tumors: diagnostically challenging areas. Mod Pathol. 2005 Feb;18 Suppl 2:S99-111.
Ruchika Garg et al (2014), studied a clinicopathological study of malignant ovarian tumors in India. JSAFOMS 2014 jan-June; 2(1), 9-11.
K. Okugawa and others, ‘Relationship between Age, Histological Type, and Size of Ovarian Tumors’, International Journal of Gynaecology and Obstetrics: The Official Organ of the International Federation of Gynaecology and Obstetrics, 74.1 (2001), 45–50.
V. McGuire and others, ‘Parity and Oral Contraceptive Use in Relation to Ovarian Cancer Risk in Older Women’, Cancer Epidemiology Biomarkers & Prevention, (2016) June, 25(7) 1059–63.
Berit Jul Mosgaard and others, impact of parity, infertility and treatment with fertility drugs on the risk of ovarian cancer. Am J Epidemiol 2002Feb 155 (3): 217-224.
Adami HO, Hsieh CC, Lambe M, Trichopoulos D, Leon D, Persson I, Ekbom A, Janson PO. Parity, age at first childbirth, and risk of ovarian cancer. Lancet. 1994 Nov 5;344(8932):1250-4.
CA Iyoke and others, ‘Incidence, Pattern and Management of Ovarian Cancer at a Tertiary Medical Center in Enugu, South East Nigeria’, Annals of Medical and Health Sciences Research, (2013) July- Sep, 3(3) 417–21.
Fatimah Zahra and others, parity and epithelial tumors, Federal Government Services Hospital, Islamabad . P J M H S 2007JAN –MAR;1(1) 45-47.
Kjaer SK, Mellemkjaer L, Brinton LA, Johansen C, Gridley G, Olsen JH. Tubal sterilization and risk of ovarian, endometrial and cervical cancer. A Danish population-based follow-up study of more than 65 000 sterilized women. Int J Epidemiol. 2004 Jun;33(3):596-602. Epub 2004 May 26.
Cibula D, Widschwendter M, Májek O, Dusek L. Tubal ligation and the risk of ovarian cancer: review and meta-analysis. Hum Reprod Update. 2011 Jan-Feb;17(1):55-67. doi: https://doi.org/10.1093/humupd/dmq030. Epub 2010 Jul 15.
Weiva Sieh and others, ‘Tubal Ligation and Risk of Ovarian Cancer Subtypes: A Pooled Analysis of Case-Control Studies’, International Journal of Epidemiology, (2013) April, 42(2) 579–89.
Hankinson SE, Hunter DJ, Colditz GA, Willett WC, Stampfer MJ, Rosner B, Hennekens CH, Speizer FE. Tubal ligation, hysterectomy, and risk of ovarian cancer. A prospective study. JAMA. 1993 Dec 15;270(23):2813-8.
Farooq S, Tasleem R, Nazir N, Reshi R, Hassan Z. HISTOPATHOLOGICAL PATTERN OF OVARIAN NEOPLASMS AND ESTROGEN AND PROGESTERONE RECEPTOR EXPRESSION IN PRIMARY EPITHELIAL TUMOURS AND THEIR HISTOPATHOLOGICAL CORRELATION. Int J Curr Res Rev. nov 2013 Nov;5(21):70–7.
Giurgea LN, Ungureanu C, Mihailovici MS. The immunohistochemical expression of p53 and Ki67 in ovarian epithelial borderline tumors. Correlation with clinicopathological factors. Rom J Morphol Embryol. 2012;53(4):967-73.
Kacar Ozkara S, Filinte D. Tp53 Expression And Ki-67 Proliferation Index In Surface Epithelial Tumors Of The Ovary And Their Relationship With The Histopathological Prognostic Parameters. Med J Trak Univ Balkan Med J 2011;28:394-408.
Daraı̈ E, Walker-Combrouze F, Dauge-Geoffroy M-C, Vincent Y, Feldmann G, Madelenat P, et al. Ki 67 expression in 35 borderline ovarian tumours: relations with clinicopathologic parameters and ploidy. Eur J Obstet Gynecol Reprod Biol. 1998 Feb 1;76(2):175–80.
Zheng W, Lu JJ, Luo F, Zheng Y, Feng Yj, Felix JC, Lauchlan SC, Pike MC. Ovarian epithelial tumor growth promotion by follicle-stimulating hormone and inhibition of the effect by luteinizing hormone. Gynecol Oncol. 2000 Jan;76(1):80-8.
van Kruchten M, van der Marel P, de Munck L, Hollema H, Arts H, Timmer-Bosscha H, de Vries E, Hospers G, Reyners A. Hormone receptors as a marker of poor survival in epithelial ovarian cancer. Gynecol Oncol. 2015 Sep;138(3):634-9. doi: https://doi.org/10.1016/j.ygyno.2015.06.032. Epub 2015 Jun 24.
Choudhury M, Goyal S, Pujani M. A cytohistological study of Ki-67 expression in ovarian tumors. Indian J Pathol Microbiol. 2011 Jan-Mar;54(1):21-4. doi: http://www.ijpmonline.org/text.asp?2011/54/1/21/77318.
Liu P, Sun YL, Du J, Hou XS, Meng H. CD105/Ki67 coexpression correlates with tumor progression and poor prognosis in epithelial ovarian cancer. Int J Gynecol Cancer. 2012 May;22(4):586-92. doi: 10.1097/IGC.0b013e31823c36b8.
Buchynska LG, Iurchenko NP, Grinkevych VM, Nesina IP, Chekhun SV, Svintsitsky VS. Expression of the estrogen and progesterone receptors as prognostic factor in serous ovarian cancers. Exp Oncol. 2009 Mar;31(1):48-51.
Arias-Pulido H, Smith HO, Joste NE, Bocklage T, Qualls CR, Chavez A, Prossnitz ER, Verschraegen CF. Estrogen and progesterone receptor status and outcome in epithelial ovarian cancers and low malignant potential tumors. Gynecol Oncol. 2009 Sep;114(3):480-5. doi: https://doi.org/10.1016/j.ygyno.2009.05.045. Epub 2009 Jun 27.
Min KW, Park MH. The Expression of c-erbB-2, EGFR, p53 and Ki-67 in Ovarian Borderline Tumors and Carcinomas of the Ovary., The Expression of c-erbB-2, EGFR, p53 and Ki-67 in Ovarian Borderline Tumors and Carcinomas of the Ovary. Korean J Pathol Korean J Pathol. 2007 Oct ;41(5):296–306.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


