Prevalence of Bronchogenic carcinoma in the North Indian Population
Abstract
Aim: This original research article aims to study the Prevalence of Bronchogenic carcinoma in the North Indian Population.
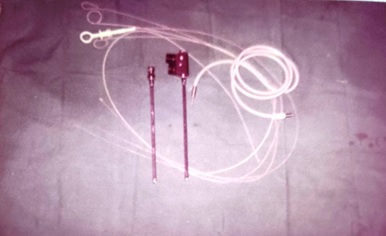
Material & Method: The present study includes 150 patients with intrathoracic space-occupying lesions, of which 42 patients with bronchogenic carcinoma were seen at SS hospital Banaras Hindu University, Varanasi, UP. Most of the patients studied were from the thoracic surgery section, while few patients were taken from other departments of SS hospital. The age of those patients varied widely, starting from 10 years to 60 years. The bulk of the patients were young adults and middle-aged persons, with 35 males and seven females. During this study, patients were investigated in systemic order with the progression of symptoms from the onset, development of latest symptoms and treatment taken before if any, history of tuberculosis, chronic cough, smoking, and contact with were recorded. The patient's vitals were recorded, and routine pathological investigation including blood count, hemoglobin and specific procedure like radiological method, sputum and bronchoscopy were performed.
Result: Maximum patients were in the age group of 41 to 50 years. Forty-two patients were diagnosed with Bronchogenic carcinoma, a definitive diagnosis was confirmed by Clinical & Radiological (chest X-ray & CT Scan) in 24 (16%), by Bronchoscopic examination & Biopsy in 15 (10%) and by thoracotomy in 03(2%). The maximum age group among the cases were 41-60. The most common symptom was Cough with expectoration in 33 patients (78.5%), followed by Haemoptysis and Dyspnea in 30 cases (71.4%). Fever was least common with 6 cases. It was observed that 18 patients (43%) had the habit of smoking for more than 18 years.
Conclusion: This study provides a framework for assessing the prevalence of bronchogenic carcinoma in the North Indian population and proves that smoking is a potential risk factor in bronchogenic carcinoma. Prevalence of Bronchogenic Carcinoma among all cases of Intrathoracic Lesions Cases 28 % and among all subjects who undergone for screening in one year – 2.84%
Downloads
References
Chalkidou K, Marquez P, Dhillon PK, Teerawattananon Y, Anothaisintawee T, Gadelha CA, Sullivan R. Evidence-informed frameworks for cost-effective cancer care and prevention in low, middle, and high-income countries. Lancet Oncol. 2014 Mar;15(3):e119-31. doi: 10.1016/S1470-2045(13)70547-3.
Sivaram S, Majumdar G, Perin D, Nessa A, Broeders M, Lynge E, et al. Population-based cancer screening programmes in low-income and middle-income countries: regional consultation of the International Cancer Screening Network in India. Lancet Oncol. 2018 Feb;19(2):e113-e122. doi: 10.1016/S1470-2045(18)30003-2.
India State-Level Disease Burden Initiative Cancer Collaborators. The burden of cancers and their variations across the states of India: the Global Burden of Disease Study 1990-2016. Lancet Oncol. 2018 Oct;19(10):1289-1306. doi: 10.1016/S1470-2045(18)30447-9.
Noronha V, Pinninti R, Patil VM, Joshi A, Prabhash K. Lung cancer in the Indian subcontinent. South Asian J Cancer. 2016 Jul-Sep;5(3):95-103. doi: 10.4103/2278-330X.187571.
Muir, Calum S., and R. G. Skeet. Cancer registration: principles and methods. Eds. Ole Møller Jensen, D. Maxwell Parkin, and Robert MacLennan. Vol. 95. Lyon: IARC, 1991.
National Centre for Disease Informatics and Research. Report on cancer burden in north eastern states of India. Bengaluru, India, national cancer registry programme (NCRP-ICMR).
Ngaihte P, Zomawia E, Kaushik I. Cancer in the NorthEast India: Where we are and what needs to be done? Indian J Public Health. 2019 Jul-Sep;63(3):251-253. doi: 10.4103/ijph.IJPH_323_18.
Pongnikorn D, Daoprasert K, Waisri N, Laversanne M, Bray F. Cancer incidence in northern Thailand: Results from six population-based cancer registries 1993-2012. Int J Cancer. 2018 May 1;142(9):1767-1775. doi: 10.1002/ijc.31203.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018 Nov;68(6):394-424. doi: 10.3322/caac.21492. Epub 2018 Sep 12. Erratum in: CA Cancer J Clin. 2020 Jul;70(4):313.
Overall evaluations of carcinogenicity: an updating of IARC Monographs volumes 1 to 42. IARC Monogr Eval Carcinog Risks Hum Suppl. 1987;7:1-440.
India State-Level Disease Burden Initiative Cancer Collaborators. The burden of cancers and their variations across the states of India: the Global Burden of Disease Study 1990-2016. Lancet Oncol. 2018 Oct;19(10):1289-1306. doi: 10.1016/S1470-2045(18)30447-9.
Gandhi AK, Kumar P, Bhandari M, Devnani B, Rath GK. Burden of preventable cancers in India: Time to strike the cancer epidemic. J Egypt Natl Canc Inst. 2017 Mar;29(1):11-18. doi: 10.1016/j.jnci.2016.08.002.
Hamilton, William Trevor. Towards earlier diagnosis of cancer in primary care: a population-based case-control study of colorectal, lung and prostate cancer. Diss. University of Bristol, 2005.
Shim J, Brindle L, Simon M, George S. A systematic review of symptomatic diagnosis of lung cancer. Fam Pract. 2014 Apr;31(2):137-48. doi: 10.1093/fampra/cmt076.
Hamilton W, Peters TJ, Round A, Sharp D. What are the clinical features of lung cancer before the diagnosis is made? A population based case-control study. Thorax. 2005 Dec;60(12):1059-65. doi: 10.1136/thx.2005.045880.
Walter FM, Rubin G, Bankhead C, Morris HC, Hall N, Mills K, Dobson C, Rintoul RC, Hamilton W, Emery J. Symptoms and other factors associated with time to diagnosis and stage of lung cancer: a prospective cohort study. Br J Cancer. 2015 Mar 31;112 Suppl 1(Suppl 1):S6-13. doi: 10.1038/bjc.2015.30.
National Cancer Intelligence Network. Routes to diagnosis. London: NCIN. p. 2015; 2016-2013 workbook [cited Aug 14 2018]. Available from: http://www.ncin.org.uk/publications/routes_to_diagnosis.
Beckett P, Tata LJ, Hubbard RB. Risk factors and survival outcome for non-elective referral in non-small cell lung cancer patients--analysis based on the National Lung Cancer Audit. Lung Cancer. 2014 Mar;83(3):396-400. doi: 10.1016/j.lungcan.2013.10.010.
Hamilton W. Cancer diagnosis in primary care. Br J Gen Pract. 2010 Feb;60(571):121-8. doi: 10.3399/bjgp10X483175.
Public Health England. Patient dose information: guidance; 2008 [cited Nov 27 2018]. Available from: https://www.gov.uk/government/publications/medical-radiation-patient-doses/patient-dose-information-guidance.
Stapley S, Sharp D, Hamilton W. Negative chest X-rays in primary care patients with lung cancer. Br J Gen Pract. 2006 Aug;56(529):570-3.
Fernández V, Alonso JL, Munuera L, Moya JL, Lasa B, Suárez A, Gutiérrez J. Análisis de los casos de cáncer de pulmón diagnosticados en el Servicio de Medicina Interna del Hospital de Navarra: enero de 2001 a septiembre de 200 [Analysis of lung cancer cases diagnosed in an internal medicine department: from January 2001 to September 2006]. An Sist Sanit Navar. 2007 Sep-Dec;30(3):353-62. Spanish. doi: 10.4321/s1137-66272007000500004.
Bjerager M, Palshof T, Dahl R, Vedsted P, Olesen F. Delay in diagnosis of lung cancer in general practice. Br J Gen Pract. 2006 Nov;56(532):863-8.
Mitchell, E., U. Macleod, and G. Rubin. "Cancer in primary care: an analysis of significant event audits (sea) for diagnosis of lung cancer and cancers in teenagers and young adults 2008-2009." (2009).
Kennedy MPT, Cheyne L, Darby M, Plant P, Milton R, Robson JM, et al. Lung cancer stage-shift following a symptom awareness campaign. Thorax. 2018 Dec;73(12):1128-1136. doi: 10.1136/thoraxjnl-2018-211842.
Athey VL, Suckling RJ, Tod AM, Walters SJ, Rogers TK. Early diagnosis of lung cancer: evaluation of a community-based social marketing intervention. Thorax. 2012 May;67(5):412-7. doi: 10.1136/thoraxjnl-2011-200714.
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


