Evaluation of Some common clinical factors in extensive vitiligo- a case control study
Abstract
Introduction: Vitiligo is a common depigmenting disorder with profound stigma. Prevalence of vitiligo is 0.5% to 1%. Information about association of progressive vitiligo are well known. Prognostic factors of vitiligo also enlisted. However, little information is available on the risk factors for developing extensive vitiligo.
Aims and Objectives: Aims of the study was to identify – factors which are associated with extensive vitiligo (involving more than 5% of the body surface area). The following risk factors were evaluated, Onset before 20 years of age, Duration of disease greater than 2 years, Presence of Koebner’s phenomenon, Family history of vitiligo, Presence of leucotrichia and Mucosal involvement.
Materials and Methods: A case control study were designed. Patients with Vitiligo > 5% body surface area involvement were classified as cases and <5% body surface area were labeled as controls. The frequency of evaluating associated clinical factors among the cases and controls were used to evaluate the extensive vitiligo’s association with risk factors (disease risk associated exposure).
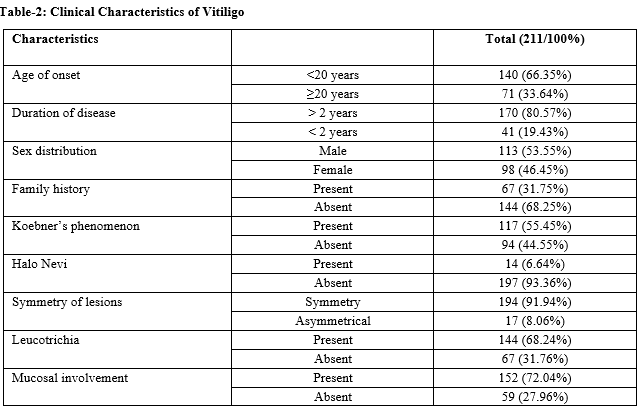
Results: Two hundred and eleven patients were evaluated. The mean age at onset was 19.07+13.51 (+SD) years. Acrofacial vitiligo was the commonest type of vitiligo. Duration of disease more than 2 years, presence of Koebner’s Phenomenon, Family history, Symmetry of lesions, milky white colour of lesion, presence of Leucotrichia, mucosal involvement and Acrofacial type vitiligo had statistically significant (p<.05) association with extensive vitiligo. Ratio of the odds of the outcomes in two groups was noted significant with Duration of disease more than 2 years, Koebner,s Phenomenon, Mucosal involvement and Leucotrichia.
Conclusion: This case-control study has demonstrated a weak association between extensive vitiligo and duration of disease greater than 2 years. It has also indicated that koebner’s phenomenon, mucosal involvement and leucotrichia are additional risk factors.
Downloads
References
Alikhan A, Felsten LM, Daly M, Petronic-Rosic V.. Vitiligo: A comprehensive overview Part II. J Am Acad Dermatol. 2011;65(3):473-491. doi: https://doi.org/10.1016/j.jaad.2010.11.061.
Zhang Y,CaiY,Shi M, Jiang S, Cui S, Wu Y et al. The Prevalence Of Vitiligo. A metaanalysis. PLoS One. 2016 Sep 27;11(9):e0163806. doi: https://doi.org/10.1371/journal.pone.0163806. eCollection 2016.
Das SK, Majumder PP, Chakraborty R, Majumdar TK, Haldar B. Studies on vitiligo I. Epidemiological profile in Calcutta, India. Genet Epidemiol. 1985;2(1):71-78. doi: https://doi.org/10.1002/gepi.1370020107.
Das SK, Majumder PP, Majumder TK, Haldar B. Studies on vitiligo II. Familial aggregation and genetics, Genet Epidemiol. 1985b;2(2):255-262. doi: https://doi.org/10.1002/gepi.1370020303.
Majumder PP, Das DK, Li CC. A genetic model for vitiligo. Am J Human Genet. 1988;43(2):119-125.
Majumder PP, Nordlund JJ, Nath SK. Pattern of familial aggregation of vitiligo. Arch Dermatol. 1993;129(8): 994-998. doi: https://dx.doi.org/10.1001/archderm.1993.01680290066010.
Hann SK, Chun WH, Park YK.Clinical characteristics of progressive vitiligo. Int J Dermatol. 1997;36(5):353-355. doi: https://doi.org/10.1046/j.1365-4362.1997.00162.x.
Du Vivier A, Disorder of pigmentation.In Du Vivier A, Mckee PH, Editors. Atlas of clinical dermatology, 2nd Edition. London: Gower Medical Publication;1992. Pp 25.8.
Dutta AK, Dutta PK, Pigmentary disorders. In Valia RG, Valia AR, editors. IADVL Textbook and Atlas of Dermatology, 1st edition. Bombay: Bhalani Publishing House: 1994. pp 500-586.
Lund CC, Browder NC. The estimation of area of burns. Surg Gynecol Obstet. 1944;7(1):352-358.
Teulings HE, Ceylan E, Overkamp M, Vrijman C, Bos JD, Nijsten TE, et al. Nonsegmental vitiligo disease duration and female sex are associated with comorbidity and disease extent: a retrospective analysis in 1307 patients aged ≥ 50 years. Br J Dermatol. 2016;175(4):821-824. doi: https://doi.org/10.1111/bjd.14640.
Van Geel N, Speeckaert R, De Wolf J, Bracke S, Chevolet I, Brochez L, et al .Clinical significance of Koebner phenomenon in vitiligo. Br J Dermatol. 2012;167(5):1017-1024. doi: https://doi.org/10.1111/j.1365-2133.2012.11158.x.
Khurrum H, AlGhamdi KM, Bedaiwi KM, AlBalahi NM. Multivariate Analysis of Factors Associated with the Koebner Phenomenon in Vitiligo: An Observational Study of 381 Patients. Ann Dermatol. 2017;29(3):302-306. doi: https://doi.org/10.5021/ad.2017.29.3.302. Epub 2017 May 11.
Shagil EM, Agarawal D, Vagadia K, Marfatia YS, Begum R. Vitiligo: clinical profiles in Vadodara, Gujrat. Indian J Dermatol. 2006;51(2):100-104. doi: http://www.e-ijd.org/text.asp?2006/51/2/100/26928.
Mahajan VK, Vashist S, Chauhan PS, Mehta KI, Sharma V, Sharma A,.clinico-epidemiological profile of patients with vitiligo: a retrospective study from a tertiary care centre of North India. Ind Dermatol Onl J. 2019;10(1):38-44. doi: https://dx.doi.org/10.4103%2Fidoj.IDOJ_124_18.
Mogawer RM, Elmasry MF, Mostafa WZ. New insights into leucotrichia in nonsegmental vitiligo: A crossesctionalstudy: Ind J Dermatol Venereol Leprol. 2019;85(4):374-379. doi: http://www.ijdvl.com/text.asp?2019/85/4/374/255790.
Sehgal VN: A clinical evaluation of 202 cases of vitiligo. Cutis. 1974:439-445.
Datta AK, Mondal SB. A clinical study of 650 vitiligo cases and their classification. Ind J Derm. 1969;14(3):103-111.
Norlund JJ. Vitiligo: A Review of Some Facts Lesser Known About Depigmentation. Indian J Dermatol. 2011;56(2):180-189. doi: https://dx.doi.org/10.4103%2F0019-5154.80413.
Goudie RB, Soukop M, Dagg JH, Lee FD. Hypothesis: Symmetrical cutaneous lymphoma. Lancet. 1990; 335(8685):316-318. doi: https://doi.org/10.1016/0140-6736(90)90607-7.
Kanwar AJ, Mahajan R, Parsad D. Effect of age at onset on disease characteristics in vitiligo. J Cutan Med Surg. 2013;17(4):253-258. doi: https://doi.org/10.2310/7750.2013.12075.
Euphemia W. Mu, Brandon E. Cohen, BS, Seth J. Orlow,. Early-onset childhood vitiligo is associated with a more extensive and progressive course. J Am Acad Dermatol. 2015;73(3):467-470. doi: https://doi.org/10.1016/j.jaad.2015.05.038.
Chun WH, Hann SK.. The progression of nonsegmental vitiligo: clinical analysis of 318 patients. Int J Dermatol. 1997;36(12):908-910. doi: https://doi.org/10.1046/j.1365-4362.1997.00320.x.
Barona MI, Arrrunatehui A: An epidemiologic case-control study in a population with vitiligo. J Am Acad Derm. 1995;33(4):621-625. doi: https://doi.org/10.1016/0190-9622(95)91282-7.
Soo Min Kim,Han-Seung Lee, Seung-Kyung Hann. The efficacy of low-dose oral corticosteroids in the treatment of vitiligo patients, Int J Dermatol. 1999;38(7):546-550. doi: https://doi.org/10.1046/j.1365-4362.1999.00623.x.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


