A study to assess the quality of life (QOL) of patients suffering from tinea corporis attending dermatology OPD of a tertiary care centre of Eastern India
Abstract
Background: A huge number of patients in our country are affected by Tinea Corporis (TC). The number of patients affected by dermatophytosis has increased by a large extent in the last 4 to 5 years. The quality of life in TC patients can be affected by various factors including the disease morbidity, duration of disease, social & demographic factors.
Aims and Objectives: The aim of the study is to find out the effect of TC on the quality of life of the affected patients & along with that to assess whether there is some association of this effect on quality of life with some demographic & clinical factors.
Methods: The effect on quality of life of 328 patients affected by TC who attended the Dermatology outpatient’s department of NRS Medical College was assessed using the Dermatology Life Quality Index (DLQI) questionnaire.
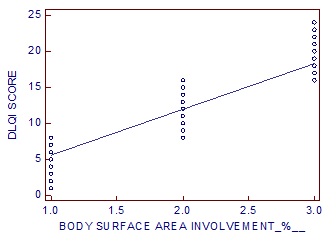
Results: 12 (3.658 %) of the patients had an extremely large effect on quality of life. There was a very large effect on the QOL of 121 (36.890 %) patients. There was moderate effect on 134 (40.853 %) of the patients. There was a small effect on 59 (17.987 %) of the patients. 2 (0.609 %) patients had no effect on their QOL. Duration of disease & body surface area involved have significant impacts on QOL.
Conclusion: The quality of life is adversely affected by TC. Early detection & treatment of the disease is very important. Steps must be taken to increase awareness about the disease among the general population.
Downloads
References
WHOQOL Group. Development of the World Health Organization WHOQOL-BREF QOL assessment. Psychol Med. 1998;28(3):551-558.
Halioua B, Bemmont MG, Lunel F. QOLin Dermatology. Int J Dermatol.2000;39:801-806.
Verma S, Madhu R. The great Indian epidemic of superficial dermatophytosis: An appraisal. Indian J Dermatol.2017;62(3):227-236. doi: https://dx.doi.org/10.4103%2Fijd.IJD_206_17.
D’Souza MJ. Awareness of Risk Factors for Dermatophytoses and its impact on QOL among adults in Mangalore. A Cross-sectional study. IOSR J Dent Med Sci (IOSR-JDMS). 2018;17(6):64-70. doi: 10.9790/0853-1706016470.
Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI): a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19(3):210-216. doi: https://doi.org/10.1111/j.1365-2230.1994.tb01167.x.
Yeung H, Takeshita J, Mehta NN, Kimmel SE, Ogdie A, Margolis DJ, et al. Psoriasis severity and the prevalence of major medical comorbidity: a population-based study. JAMA Dermatol.2013;149(10):1173-1179. doi: https://dx.doi.org/10.1001/jamadermatol.2013.5015.
Dogra S, Narang T. Emerging atypical and unusual presentations of dermatophytosis in India. Clin Dermatol Rev. 2017;1(3):12-18. doi: http://www.cdriadvlkn.org/text.asp?2017/1/3/12/216277.
Weitzman I, Summerbell RC. The dermatophytes. Clin Microbiol Rev. 1995;8(2):240-259. doi: https://dx.doi.org/10.1128/CMR.8.2.240.
Sahoo AK, Mahajan R. Management of tinea corporis, tinea cruris, and tinea pedis: A comprehensive review. Indian Dermatol Online J. 2016;7(2):77-86. doi: https://dx.doi.org/10.4103%2F2229-5178.178099.
Patro N, Panda M, Jena AK. The Menace of Superficial Dermatophytosis on the QOLof Patients Attending Referral Hospital in Eastern India: A Cross-sectional Observational Study. Indian Dermatol Online J. 2019;10(3):262-266. doi: https://dx.doi.org/10.4103%2Fidoj.IDOJ_342_18.
Dogra S, Uprety S. The menace of chronic and recurrent dermatophytosis in India: Is the problem deeper than we perceive? Indian Dermatol Online J. 2016;7(2):73-76. doi: https://dx.doi.org/10.4103%2F2229-5178.178100.
Panda S, Verma S. The menace of dermatophytosis in India: The evidence that we need. Indian J Dermatol Venereol Leprol. 2017;83(3):281-284. doi: http://www.ijdvl.com/text.asp?2017/83/3/281/203250.
Mohanty JC, Mohanty SK, Sahoo RC, Sahoo A, Praharaj N. Incidence of dermatophytosis in Orissa. Indian J Med Microbiol .1998;16(2):78-80.
Singh S, Beena PM. Profile of dermatophyte infections in Baroda. Indian J Dermatol Venereol Leprol. 2003;69(4):281-283.
Bindu V, Pavithran K. Clinico-mycological study of dermatophytosis in Calicut. Indian J Dermatol Venereol Leprol. 2002;68(5):259-261.
Peerapur BV, Inamdar AC, Pushpa PV, Srikant B. Clinicomycological study of dermatophytosis in Bijapur. Indian J Med Microbiol. 2004;22(4):273-274.
Sahoo AK, Mahajan R. Management of tinea corporis, tinea cruris, and tinea pedis: A comprehensive review. Indian Dermatol Online J. 2016;7(2):77-86. doi: 10.4103/2229-5178.178099.
Rajashekar TS, Nandigonnanavar S, Kuppuswamy SK, Madhavi GS. Dermatology life quality index in patients with persisting and recurrent dermatophytoses. Int J Res Dermatol. 2019;5(1):139-143. doi: http://dx.doi.org/10.18203/issn.2455-4529.IntJResDermatol20190233.
Abedini R, Hallaji Z, Lajevardi V, Nasimi M, Khaledi MK, Tohidinik HR. Quality of life in mild and severe alopecia areata patients. Int J Womens Dermatol. 2018;4(2):91-94. doi: https://doi.org/10.1016/j.ijwd.2017.07.001. eCollection 2018 Jun.
Al-Mutairi N, Eldin ON. Clinical profile and impact on quality of life: Seven years experience with patients of alopecia areata. Indian J Dermatol Venereol Leprol. 2011;77(4):489-493. doi: http://www.ijdvl.com/text.asp?2011/77/4/489/82411.
Zhang M, Zhang N. Quality of life assessment in patients with alopecia areata and androgenetic alopecia in the People’s Republic of China. Dovepress. 2017;11:151-155. doi: https://dx.doi.org/10.2147%2FPPA.S121218. eCollection 2017.
Hazarika N, Rajaprabha RK. Assessment of life quality index among patients with acne vulgaris in a suburban population. Indian J Dermatol. 2016;61(2):163-168. doi: https://dx.doi.org/10.4103%2F0019-5154.177758.
Raddadi AA, Jfri A, Samarghandi S, Matury N, Habibullah T, Alfarshoti M, et al. Psoriasis: correlation between severity index (PASI) quality of life index (DLQI) based on type of treatment. J Dermatol Surg. 2016;20(1):15-18. doi: https://doi.org/10.1016/j.jdds.2015.05.002.
Nayak PB, Girisha BS, Noronha TM. Correlation between disease severity, family income, and quality of life in psoriasis: A study from South India. Indian Dermatol Online J. 2018;9(3):165-169. doi: https://dx.doi.org/10.4103%2Fidoj.IDOJ_250_17.
Hedayat K, Karbakhsh M, Ghiasi M, Goodarzi A, Fakour Y, Akbari Z, et al. Quality of life in patients with vitiligo: a cross-sectional study based on Vitiligo Quality of Life index (VitiQoL). Health Qual Life Outcomes. 2016;14:1-9. doi: https://doi.org/10.1186/s12955-016-0490-y.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


