Left ventricular dysfunction in chronic obstructive pulmonary disease
Abstract
Introduction: The prevalence of LV dysfunction is probably high in COPD patients because this condition shares common risk factors.The diagnosis of left heart failure is difficultin the early phases of COPD and also during exacerbation due to similarities in signs and symptoms. Bio-markers like hsCRP is found to be elevated in stable phase as well as in exacerbation of COPD.
Objectives: To assess LV Dysfunction(Systolic and Diastolic) and to correlate Age, Symptoms, Duration and stage of illness, CRP with LV Dysfunction.
Methods: Total 100 patients of which 50 were age and sex matched controls not having COPD complying with Inclusion and Exclusion Criteria. After taking history and clinical examination they were evaluated for COPD and Left ventricular Dysfunction using PFT and Echocardiogram.
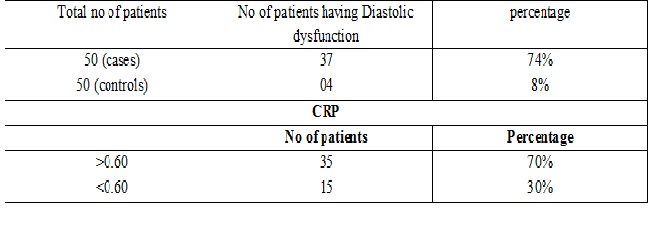
Results: Out of 50 patients, 37 patients (74%) had Diastolic dysfunction, of them 2 patients hadSystolic dysfunction also. 13 patients were normal.In the control group only 4 had Diastolic Dysfuncion.CRP was high in 35% (70%) of patients. In the higher age group of 50-60 years Diastolic dysfunction was significant. In patients of GOLD stage IV 5 out of 5 patients (100%) whereas in GOLD stage I and II it was in 1 case (16.66%) and21 case (80.76%) respectively. While comparing with the control group incidence of LV dysfunction parameters and CRP is more in case group.
Conclusion: There is increased incidence ofLV Diastolic dysfunction and also with advanced GOLD stage.CRP also correlates well LVDD. Therefore it is pertinent to explore LVDD in all patients with acute exacerbation of COPD and advanced disease stage.
Downloads
References
Pauwels RA, Rabe KF. Burden and clinical features of chronic obstructive pulmonary disease (COPD). Lancet. 2004 Aug 14-20;364(9434):613-20.
Miravitlles M, Murio C, Guerrero T, Gisbert R; DAFNE Study Group. DecisionessobreAntibioticoterapia y Farmacoeconomíaen la EPOC. Pharmacoeconomic evaluation of acute exacerbations of chronic bronchitis and COPD. Chest. 2002 May;121(5):1449-55.
Anthonisen NR, Manfreda J, Warren CP, et al. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med. 1987 Feb;106(2):196-204.
Yang S, Tan KL, Devanand A, et al. Acute exacerbation of COPD requiring admission to the intensive care unit. Respirology. 2004 Nov;9(4):543-9. DOI: https://doi.org/10.1111/j.1440-1843.2004.00615.x.
Wang CS, FitzGerald JM, Schulzer M, et al. Does this dyspneic patient in the emergency department have congestive heart failure? JAMA. 2005 Oct 19;294(15):1944-56. DOI: https://doi.org/10.1001/jama.294.15.1944.
Sin DD, McAlister FA, Man SF, Anthonisen NR. Contemporary management of chronic obstructive pulmonary disease: scientific review. JAMA. 2003 Nov 5;290(17):2301-12. DOI: https://doi.org/10.1001/jama.290.17.2301.
Remes J, Miettinen H, Reunanen A, Pyörälä K. Validity of clinical diagnosis of heart failure in primary health care. Eur Heart J. 1991 Mar;12(3):315-21.
Wheeldon NM, MacDonald TM, Flucker CJ, et al. Echocardiography in chronic heart failure in the community. Q J Med. 1993 Jan;86(1):17-23.
Render ML, Weinstein AS, Blaustein AS. Left ventricular dysfunction in deteriorating patients with chronic obstructive pulmonary disease. Chest l995:107:162 – l68.
McCllough PA, Hollander JE, Nowak RM, Storrow AB, Duc P, Omland T, McCord J, Herrmann HC, Steg PG, Westheim A, Knudsen LW, Abraham WT, Lamba S, Wu AH, Perez A, Clopton P, Krishnaswany P, Kazanegra R, Maisel AS. Uncovering heart failure in patients with a history of pulmonary disease: rationale for the early use of B-type natriuretic peptide in the emergency department. AcadEmerg Med 2003; 10: 198 – 204.
Maisel A, Hollander JE, Guss D, et al. Primary results of the Rapid Emergency Department Heart Failure Outpatient Trial (REDHOT). A multicenter study of B-type natriuretic peptide levels, emergency department decision making, and outcomes in patients presenting with shortness of breath. J Am Coll Cardiol. 2004 Sep 15;44(6):1328-33. DOI: https://doi.org/10.1016/j.jacc.2004.06.015.
Maisel AS, Krishnaswamy P, Nowak RM, et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med. 2002 Jul 18;347(3):161-7. DOI: https://doi.org/10.1056/NEJMoa020233.
Maisel AS. The diagnosis of acute congestive heart failure: role of BNP measurements. Heart Fail Rev. 2003 Oct;8(4):327-34.
Januzzi JL Jr, Camargo CA, Anwaruddin S, et al. The N-terminal Pro-BNP investigation of dyspnea in the emergency department (PRIDE) study. Am J Cardiol. 2005 Apr 15;95(8):948-54. DOI: https://doi.org/10.1016/j.amjcard.2004.12.032.
McCullough PA, Nowak RM, McCord J, Hollandcr JE, Herrmann HC, Steg PG, Duc P, Westheim A, Omland T, Knudsen CW et al. B-type natriuretic peptide and clinical judgment in emergency diagnosis of heart failure: analysis from Breathing Not Properly (BNP) Multinational Study. Circulation 2002; 106: 416 – 422.
Cabanes L, Richaud-Thiriez B, Fulla Y, Heloire F, Vuillemard C, Weber S, Dusser D. Brain natriuretic peptide blood levels in the differential diagnosis dyspnea. Chest 2001; 120: 2047—2051.
Yap LB, Mukherjee D, Timms PM, Ashrafian H. Coghlan JG. Natriuretic peptides, respiratory disease and the right heart. Chest 2004; l26: 1330 – 1336.
Phua J, Lim TK, Lee KH. B-type natriuretic peptide: issues for the intensivist and pulmonologist. Crit Care Med. 2005 Sep;33(9):2094-13.
Light RW, George RB. Serial pulmonary function in patients with acute heart failure. Arch Intern Med. 1983 Mar;143(3):429-33.
Cabanes LR, Weber SN, Matran R, et al. Bronchial hyperresponsiveness to methacholine in patients with impaired left ventricular function. N Engl J Med. 1989 May 18;320(20):1317-22. DOI: https://doi.org/10.1056/NEJM198905183202005
Pison C, Malo JL, Rouleau JL, Chalaoui J, Ghezzo H, Malo J. Bronchial hyperresponsiveness to inhaled methacholine in subjects with chronic left heart failure at time of exacerbation and after increasing diuretic therapy. Chest 1989; 96: 230 – 35.
Wijnhoven HA, Kriegsman DM, HesselinkAE, et al. Determinants of different dimensions of disease severity in asthma and COPD : pulmonary function and health-related quality of life. Chest. 2001 Apr;119(4):1034-42.
Singh SJ, Sodergren SC, Hyland ME, et al. A comparison of three disease-specific and two generic health-status measures to evaluate the outcome of pulmonary rehabilitation in COPD. Respir Med. 2001 Jan;95(1):71-7. DOI: https://doi.org/10.1053/rmed.2000.0976.
Herlitz J, Wiklund I, Sjoland H, Karlson BW, Karlsson T, Haglid M, et al. Relief of symptoms and improvement of quality of life five years after coronary artery bypass grafting in relation to preoperative ejection fraction. Qual Life Res 2000; 9: 467-476.
Arnold R, Ranchor AV, Koëter GH, et al. Consequences of chronic obstructive pulmonary disease and chronic heart failure: the relationship between objective and subjective health. Soc Sci Med. 2005 Nov;61(10):2144-54. DOI: https://doi.org/10.1016/j.socscimed.2005.04.025.
Rector TS, Anand IS, Cohn JN. Relationships between clinical assessments and patients' perceptions of the effects of heart failure on their quality of life. J Card Fail. 2006 Mar;12(2):87-92. DOI: https://doi.org/10.1016/j.cardfail.2005.10.002.
Funk GC, Lang I, Schenk P, et al. Left ventricular diastolic dysfunction in patients with COPD in the presence and absence of elevated pulmonary arterial pressure. Chest. 2008 Jun;133(6):1354-1359. doi: https://doi.org/10.1378/chest.07-2685. Epub 2008 Mar 13.
Suchoń E, Tracz W, Podolec P, Pieculewicz M, Płazak W, Prokop A, Nalepa P. Evaluation of Left ventricular function in patients with Chronic obstructive pulmonary disease. Pol Arch Med Wewn 2007 March;117(3):86-90.
A.K. Poddar, B.N. Chakraborti, J.L. Ghosh, S. Nandy and S. Hazra.Assessment of Left ventricular function in patients of Chronic obstructive pulmonary disease .Indian Journal of Tuberculosis 1997 Oct;44(4): 181-3.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


