Biochemical and clinical variations among severe Plasmodium Vivax malaria cases: A prospective study
Abstract
Context: Plasmodium vivax is geographically widely distributed with up to 2.5 billion people at risk and an estimated 70-80 million cases every year. India contributes 77% of the total malaria in Southeast Asia. Retrospective analysis of burden of malaria showed that disability adjusted life years due to malaria were 1.86 million years. According to recent study, West Bengal contributes 11% of total malaria cases in country and is one of states where falciparum resistance to chloroquine has been confirmed.
Aims: The aim of this study was to evaluate the biochemical and clinical profile of severe and non-severe Plasmodium vivax malaria and the complications and outcome of P. vivax malaria infections as there is very limited information on age and sex specific seasonal prevalence of malaria in different paradigms in the country.
Materials and Methods: A hospital based prospective study was conducted in Medical College, Kolkata comprising of 138 patients with fever (≥37.5˚C), peripheral smear and/or rapid diagnostic tests positive for P. vivax. Previously established cases of CKD, hematological abnormalities, chronic liver diseases and neuro-psychiatric disorders were excluded from our study. Demographical, clinical and laboratory parameters including liver function test, renal function test were documented and were presented in tabular and statistical means.
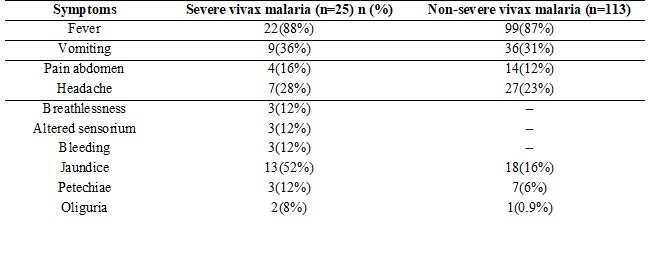
Results: Jaundice was present in 22% of patients and vomiting in 32% of the patients. Hepatomegaly was seen in 16 % cases and 33% cases had splenomegaly. ARDS was seen in 16% of severe malaria cases. Acute kidney injury was seen in 8% and cerebral malaria was seen in 12% of severe malaria cases. Multi organ dysfunction was seen in12 %cases. There was 1 death in the study due to multi organ dysfunction.
Conclusion: Life threatening complications such as ARDS, AKI, cerebral malaria and MODS can be seen in P. vivax mono infections.
Downloads
References
Garcia LS. Malaria. Clin Lab Med. 2010 Mar;30(1):93-129. doi: https://doi.org/10.1016/j.cll.2009.10.001.
Guidelines for diagnosis and treatment of malaria nvbdcp 2011.
Price RN, Douglas NM, Anstey NM. New developments in Plasmodium vivax malaria: severe disease and the rise of chloroquine resistance. Curr Opin Infect Dis. 2009 Oct;22(5):430-5. doi: https://doi.org/10.1097/QCO.0b013e32832f14c1.
Ric NP, Emiliana T, Carlos AG, et al. Vivax Malaria neglected and not benign. American journal of tropical medicine and hygiene.2007; 77:79- 87.
Bhattacharjee P, Dubey S, Gupta VK, et. al. The clinicopathologic manifestations of plasmodium vivax malaria in children: A growing menace. Journal of Clinical and Diagnostic Research.2013; 7: 861-67.
WHO. World Malaria report 2013
Guidelines for The Treatment of Malaria, WHO, 2015, 3rd edition.
Kochar DK, Das A, Kochar SK, et al. Severe Plasmodium vivax malaria: a report on serial cases from Bikaner in northwestern India. Am J Trop Med Hyg. 2009 Feb;80(2):194-8.
Farogh A, Qayyum A, Haleem A, et al. Hematological abnormality in malaria. Biomedica vol.25, Jan-Jun.2009, 52-55
Muddaiah M, Prakash PS. A study of clinical profile of malaria in a tertiary referral centre in South Canara. J Vector Borne Dis. 2006 Mar;43(1):29-33.
Bashawri LA, Mandil AA, Bahnassy AA, Ahmed MA. et al. Malaria: hematological aspects. Ann Saudi Med. 2002 Sep-Nov;22(5-6):372-6.
Jadhav UM, Patkar VS, Kadam NN. Thrombocytopenia in malaria--correlation with type and severity of malaria. J Assoc Physicians India. 2004 Aug;52:615-8.
Suman Panwar, Rajendra Kumar Soni, Nishat Ahmed. Study of epidemiological profile, clinico-biochemical spectrum and prognosis of malaria induced renal dysfunction in paediatrics age group. International Journal of Contemporary Pediatrics 2016 Feb;3(1):91-95
Edoardo G. Giannini, Roberto Testa, and Vincenzo Savarino. Liver enzyme alteration: a guide for clinicians. CMAJ. 2005 Feb 1; 172(3): 367–379.
Naha K, Dasari S, Prabhu M. Spectrum of complications associated with Plasmodium vivax infection in a tertiary hospital in South-Western India. Asian Pac J Trop Med. 2012 Jan;5(1):79-82. doi: https://doi.org/10.1016/S1995-7645(11)60251-4.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


