Contrast-enhanced ultrasound for the evaluation of hepatic artery occlusion after liver transplantation
Abstract
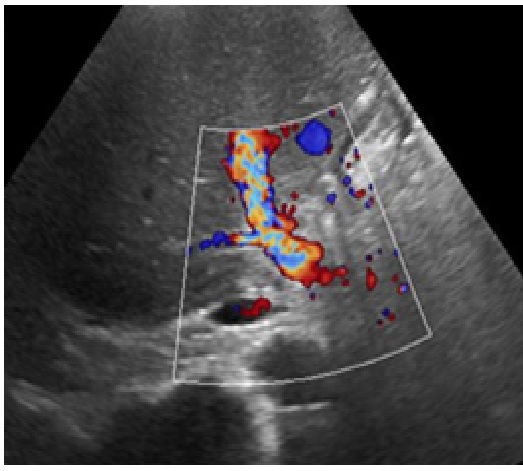
Introduction:Vascular complications after liver transplantation remain a major threat to the survival of recipients.HAT is a major cause of graft loss and patient mortality, with an incidence between 3% to 8% in transplant recipients.Early detection of HAT is critical because urgent revascularization is required to avoid severe graft loss. Although ultrasound is the preferred first-line imaging modality in patients with suspected HAT, the accuracy and positive predictive value of HAT on Doppler US are reported to be low. Moreover, Doppler examination of the hepatic vasculature is time consuming and requires a high level of operator skill. Conventional angiography remains the gold standard for diagnosis. Recently, contrast-enhanced ultrasound (CEUS) has begun providing real-time angiographic-like images of vessels at bed side and allowing the accurate diagnosis of arterial diseases such as hepatic artery thrombosis. The purpose of this study was to evaluate the efficacy of CEUS in detecting HAT after liver transplantation:
Materials and Methods: This is a retrospective data of the medical records of patients undergoing Liver transplantation in the Osmania General Hospital, Hyderabad between 2016 to 2018. Status of hepatic vascular assessment following liver transplantation done by conventional Doppler Ultra sonography and Contrast Enhanced Ultrasonography tests were obtained from registries of medical records.
Results:23 cases of post Liver transplantation aged between 4years and 58 years, with a median age of 30 years were included in the analysis. There were 20 males and 3 females. 14 patients underwent DDLT, 7 patients underwent LDLT, 1underwent split Liver transplantation and another 1 patient underwent Auto liver transplantation. Doppler US was inconclusive regarding patency of the hepatic artery (HA) circulation in 5 (21.7 %) of 23 transplantations. CEUS was performed in these 5 patients and detected HA thrombosis (HAT) in 2 cases and patent HA in 3 transplants. These 5 Transplants were confirmed by CT Angiography /conventional Angiography. In the subset of transplantations examined with CEUS, the sensitivity, specificity and accuracy of CEUS were 100%. CEUS was done at bedside without any Radiation and Nephro toxicity. In approximately 21.7% of cases, conventional Doppler US did not provide sufficient visualization of the HA after liver transplantation. In these cases, correct diagnosis was achieved by supplementary CEUS.
Conclusion:CEUS may be a new approach for early diagnosis of postoperative vascular complications after Liver Transplantation, and it can be performed at the bedside. It is safe will not cause any nephron toxicity and Radiation. CEUS is a fast, non-ionizing imaging modality for the initial exclusion of vascular complications after liver transplantation. CEUS shows a high specificity and PPV in the detection of vascular complications. In unclear cases CT still is considered as the gold standard
Downloads
References
Caiado AH, Blasbalg R, Marcelino AS, et al. Complications of liver transplantation: multimodality imaging approach. Radiographics 2007; 27: 1401.
Glockner JF, Forauer AR. Vascular or ischemic complications after liver transplantation. DOI: https://doi.org/10.2214/ajr.173.4.10511177
Flint EW, Sumkin JH, Zajko AB, Bowen A. Duplex sonography of hepatic artery thrombosis after liver transplantation. DOI: https://doi.org/10.2214/ajr.151.3.481
Hom BK, Shrestha R, Palmer SL, et al. Prospective evaluation of vascular complications after liver transplantation: comparison of conventional and microbubble contrast-enhanced US. DOI: https://doi.org/10.1148/radiol.2411050597.
Jain A, Reyes J, Kashyap R, et al. Long-term survival after liver transplantation in 4,000 consecutive patients at a single center. Ann Surg. 2000 Oct;232(4):490-500.
Sidhu PS, Shaw AS, Ellis SM, et al. Microbubble ultrasound contrast in the assessment of hepatic artery patency following liver transplantation: role in reducing frequency of hepatic artery arteriography. DOI: https://doi.org/10.1007/s00330-003-1981-x.
Vaidya S, Dighe M, Kolokythas O, Dubinsky T. Liver transplantation: vascular complications. DOI: https://doi.org/10.1097/ruq.0b013e31815d6e1d.
Horrow MM, Blumenthal BM, Reich DJ, Manzarbeitia C. Sonographic diagnosis and outcome of hepatic artery thrombosis after orthotopic liver transplantation in adults. DOI: https://doi.org/10.2214/AJR.07.2217
Crossin JD, Muradali D, Wilson SR. US of liver transplants: normal and abnormal. DOI: https://doi.org/10.1148/rg.235035031.
Defrancq J, Trotteur G, Dondelinger RF. Duplex ultrasonographic evaluation of liver transplants. Acta Radiol. 1993 Sep;34(5):478-81.
Sidhu PS, Marshall MM, Ryan SM, Ellis SM. Clinical use of Levovist, an ultrasound contrast agent, in the imaging of liver transplantation: assessment of the pre- and post-transplant patient. DOI: https://doi.org/10.1007/s003309900117
Berry JD, Sidhu PS. Microbubble contrast-enhanced ultrasound in liver transplantation. Eur Radiol. 2004 Oct;14 Suppl8:P96-103.
Marshall MM, Beese RC, Muiesan P, et al. Assessment of portal venous system patency in the liver transplant candidate: a prospective study comparing ultrasound, microbubble-enhanced colour Doppler ultrasound, with arteriography and surgery. DOI: https://doi.org/10.1053/crad.2001.0839.
Nolten A, Sproat IA. Hepatic artery thrombosis after liver transplantation: temporal accuracy of diagnosis with duplexUS and the syndrome of impending thrombosis. DOI: https://doi.org/10.1148/radiology.198.2.8596865
Hirota M, Kaneko T, Sugimoto H, et al. Intrahepatic circulatory time analysis of an ultrasound contrast agent in liver cirrhosis. Liver Int 2005; 25: 337.
Dydynski PB, Bluth EI, Altmeyer W, et al. Collateral transformation of the hepatic artery after liver transplantation. DOI: https://doi.org/10.2214/AJR.07.3625.
Dodd GD 3rd, Memel DS, Zajko AB, et al. Hepatic artery stenosis and thrombosis in transplant recipients: Doppler diagnosis with resistive index and systolic acceleration time. DOI: https://doi.org/10.1148/radiology.192.3.8058930
Hariharan Y, Makuuchi M, Takayama T, Kawarasaki H, Kubota K, Ito M, Tanaka H, Aoyanagi N, Matsukura A, Kita Y, Saiura A, Sakamoto Y, Kobayashi T, Sano K, Hashizume K, Nakatsuka T. Arterial waveforms on Doppler ultrasonography predicting or supporting hepatic arterial thrombosis in liver transplantation. Transplant Proc 1998; 30: 3188-3189 [PMID: 9838409 DOI: https://doi.org/10.1016/s0041-1345(98)00988-9.
Herold C, Reck T, Ott R, et al. Contrast-enhanced ultrasound improves hepatic vessel visualization after orthotopic liver transplantation. DOI: https://doi.org/10.1007/s00261-001-0064-1
Lu Q, Zhong XF, Huang ZX, et al. Role of contrast-enhanced ultrasound in decision support for diagnosis and treatment of hepatic artery thrombosis after liver transplantation. DOI: https://doi.org/10.1016/j.ejrad.2011.11.015


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


