Clinico-Microbiological profile in dacryocystitis: a prospective observational study
Abstract
Introduction: Dacryocystit is is the inflammatory condition of the lacrimal sac which occur in acute and chronic form. Chronic dacryocystitis is commonly encountered, accounting for 87.1% of Epiphorawhich causes social embarrassment due to chronic watering from the eye. Understanding the antibiogram for micro organism causing inflammation of lacrimal sac can be useful in choosing the best antimicrobial. Hence the present study was done to evaluate the clinical profile and antibiogram of acute and chronic dacryocystitis.
Method: A prospective observational study was done in patients with acute or chronic dacryocystitis attending ophthalmology OPD. Those fulfilling the eligibility criteria were enrolled in the study. Samples were collected from all the cases and were sent to microbiology lab for gram staining, culture and sensitivity.
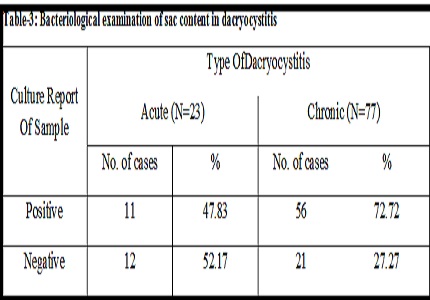
Result: 100 patients of dacryocystitis were enrolled, chronic dacryocystitis was found common than the acute dacryocystitis, along with a female (middle age group) preponderance. The main presenting symptom was watering (89%) followed by discharge (47%), swelling (34%), pain (23%) and tenderness (23%). Gram positive organisms (72.86%) were most commonly isolated. Among the Gram-positive organisms, Staph. aureus (37.14%) while Pseudomonas among Gram negative were the common isolate. Vancomycin and tobramycin are highly active against all Gram positive, tobramycin, gentamycin, fluoroquinolones and cephalosporins are found to be very active against Gram negative bacteria.
Conclusion: The most common bacterial isolate in dacryocystitis, prevailing in this geographical area is Staphylococcus (Gram positive) followed by Pseudomonas, Pneumococcus and Staph epidermidis. Combination of Vancomycin and 3rd generation cephalosporin can be used as empirical therapy when the culture reports are awaited.
Downloads
References
Disease of the Lacrimal Apparatus. In Parson;s Diseases of the Eye: Sihota R, Tandon R editors.Elsevier ,New delhi.2007;20th Ed:pp 444-452.
Eshraghi B, Abdi P, Akbari M, Fard MA. Microbiologic spectrum of acute and chronic dacryocystitis. International journal of ophthalmology. 2014;7(5):864.
JACOBS HB. Symptomatic epiphora. Br J Ophthalmol. 1959 Jul;43:415-34.
Mandal R, Banerjee AR, Biswas MC, Mondal A, Kundu PK, Sasmal NK. Clinicobacteriological study of chronic dacryocystitis in adults. Journal of the Indian Medical Association. 2008 ;106(5):296-8.
Ali MJ, Joshi SD, Naik MN, Honavar SG. Clinical profile and management outcome of acute dacryocystitis: two decades of experience in a tertiary eye care center. SeminOphthalmol. 2015 Mar;30(2):118-23. doi: https://doi.org/10.3109/08820538.2013.833269. Epub 2013 Oct 30.
Mills DM, Bodman MG, Meyer DR, MortonAD 3rd; ASOPRSDacryocystitisStudy Group. The microbiologicspectrum of dacryocystitis: a nationalstudy of acuteversuschronicinfection. OphthalmicPlastReconstr Surg.2007 Jul-Aug;23(4):302-6.
Chaudhry IA, Shamsi FA, Al-RashedW. Bacteriology of chronic dacryocy stitisinatertiary eye care center. Ophthalmic Plast Reconstr Surg. 2005 May;21(3):207-10.
Huber-Spitzy V, Steinkogler FJ, Huber E, Arocker-Mettinger E, Schiffbänker M. Acquired dacryocystitis: microbiology and conservative therapy. Acta Ophthalmol (Copenh). 1992 Dec;70(6):745-9.
Sun X, Liang Q, Luo S, Wang Z, Li R, Jin X. Microbiological analysis of chronic dacryocystitis. Ophthalmic and Physiological Optics. 2005;25(3):261-3.
Ramesh S, Ramakrishnan R, Bharathi MJ, Amuthan M, Viswanathan S.Prevalence of bacterial pathogens causingocular infections in South India. Indian J Pathol Microbiol. 2010 Apr-Jun;53(2):281-6. doi: http://www.ijpmonline.org/text.asp?2010/53/2/281/64336.
Amin RM, Hussein FA, Idriss HF, Hanafy NF, Abdallah DM. Pathological, immunohistochemical and microbiologicalal analysis of lacrimal sac biopsies in patients with chronic dacrocystitis. International journal of ophthalmology. 2013;6(6):817-26.
Sharma S.Antibiotic resistance in ocularbacterialpathogens. Indian J Med Microbiol. 2011 Jul-Sep;29(3):218-22. doi: http://www.ijmm.org/text.asp?2011/29/3/218/83903.
Modarrres SH, LasheiiA , Nassiri ON. Bacterial etiologic agents of ocular infection in children in the Islamic Republic of Iran. 1998;4(1):44-49.
Bharathi MJ, Ramakrishnan R, Maneksha V, Shivakumar C, Nithya V, Mittal S. Comparative bacteriology of acute and chronic dacryocystitis. Eye (Lond). 2008 Jul; 22(7):953-60. Epub 2007 Jun 29.
Prakash R., GirishBabu R.J., Nagaraj E.R., Prashanth H.V., Jayashree S. Shah. A bacteriological study of dacryocystitis. Journal Of Clinical And Diagnostic Research 2012 ; 6(4):652-655.
Rizvi SA, Rizvi M, Raut SD, Gupta Y, Maheshwari P. Etiology and antimicrobial sensitivity pattern in acute and chronic dacryocystitis. International Journal of Current Microbiology and Applied Sciences: ISSN: 2319-7706 Special Issue-1 (2015) pp. 269-280.
Shah CP, Santani D. A comparativebacteriologicalprofile and antibiogram of dacryocystitis. Nepal J Ophthalmol. 2011 Jul-Dec;3(2):134-9. doi: http://dx.doi.org/10.3126/nepjoph.v3i2.5265.
Kandati J, Kumar GK, Avanish G, Buchineni M, Mohan R, Pathapati PS. Microbial surveillance of acute and chronic dacryocystitis in a tertiary care hospital. Journal of Evolution of Medical and Dental Sciences. 2015;4(3):408-16.
Diggle FH.LacrymalObstruction: Its NasalOrigin and IntranasalTreatment. Br Med J.1927 Nov 19;2(3489):933-5.
REDDY PS, REDDY B. Dacryocystitis; a clinico-pathologicalstudy.J Indian Med Assoc.1955 Mar 1;24(11):413-6.
Chaudhary M, Bhattarai A, Adhikari SK, Bhatta DR.Bacteriology and antimicrobialsusceptibility of adultchronicdacryocystitis. Nepal J Ophthalmol. 2010 Jul-Dec;2(2):105-13. doi: https://doi.org/10.3126/nepjoph.v2i2.3716
Sarkar I, Choudhury SK, Bandyopadhyay M, Sarkar K, Biswas J. A Clinicobacteriological Profile Of Chronic Dacryocystitis In Rural India. International journal of Health Science and Research 2015;5(7):82-87.
Kalaivani K. Microbial Study Of Chronic Dacryocystitis In Adults. International Journal of Ocular Oncology and Oculoplasty. 2017;3(2):133-136.
Katre P, Harkare V. Epidemiological Study OfDacryocystitis In Rural Population. Panacea Journal Of Medical Sciences. 2017 ;7(1):11-4.
Patel K, Magdum R, Sethia S, Lune A, Pradhan A, Misra RN. A Clinico-Bateriological Study Of Chronic Dacryocystitis. Sudanese Journal Of Ophthalmology. 2014 ;6(1):1-5.
Sharat S, Nagaraja KS. A Study On The Epidemiology Of Chronic Dacryocystitis In An Economically-Deprived Population In South India. Journal of evolution of medical and dental sciences-jemds. 2016;5(70):5116-7.
Malik SR, Gupta AK, Chaterjee S, Bhardwaj OP, Saha M. Dacryocystography of normal and pathological lacrimal passages. Br J Ophthalmol. 1969 Mar;53(3):174-9.
Mandal R, Banerjee AR, Biswas MC, Mondal A, Kundu PK, Sasmal NK. Clinicobacteriological Study Of Chronic Dacryocystitis In Adults. Journal Of the Indian Medical Association. 2008;106(5):296-8.
Kubravi SH, Qureshi ST, Akbar E, Nawaz S, Kawoosa K. Characteristics And Surgical Outcomes Of Patients Undergoing Dacryocystorhinostomy In Kashmir. Journal of evolution of medical and dental sciences. 2016;5(93):6879-82.
Das JK, Deka AC, Kuri GC, Bhattacharjee K, Das D, Gogoi K. Bacteriology of chronic dacryocystitis in adult population of northeast India. Orbit. 2008;27(4):243-7. doi: https://doi.org/10.1080/01676830802224668.
Ahuja S, Chhabra AK, Agarwal J. Study Of Bacterial Spectrum In Patients Of Chronic Dacryocystitis, At A Tertiary Care Centre In Northern India. J Community Med Health Educ2017;7:536.doi: https://doi.org/10.4172/2161-0711.1000536.
Ali MJ, Motukupally SR, Joshi SD, Naik MN. The microbiological profile of lacrimal abscess: two decades of experience from a tertiary eye care center. Journal of ophthalmic inflammation and infection. 2013;3(1):57.doi: https://doi.org/10.1186/1869-5760-3-57.
Gupta S, Gupta S, Mahajan B. Bacteriology of Acquired DacryocystitisinA Tertiary Care Hospital of North India.JK Science Journal of Medical Science and Research 2014;16(3):110-113.
Chandra TJ, Satish K, Raj RS, Sharma YV. Isolation Of Dacrocystitis Causing Bacteria Among The Patients Of East Godavari District, Andhra Pradesh. Bangladesh Journal Of Medical Science. 2016;15(3):399-402.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


