Role of trans rectal and scrotal ultra sonography in male infertility
Abstract
Introduction: Investigation of male infertility is assuming greater importance with male factors implicated as the cause in up to half of the infertile couples. This prospective cross-sectional study aims to establish the role of transrectal and scrotal ultrasonography in male infertility. Besides routine investigations trans rectal and scrotal ultra sonography was performed to detect testicular and post-testicular etiology or abnormality.
Aims: The aim of this cross-sectional study was to determine the role of transrectal and scrotal ultrasonography in the evaluation of male infertility and to compare the findings of ultrasonography with clinical and surgical findings.
Material and Methods: The prospective cross-sectional study was carried out on 50 patients visiting the ultrasound section of Rajindra Hospital; Patiala with complaint of infertility over the span of 2 years. All the patient undergoes transrectal and scrotal ultrasonography with high frequency transducer having a frequency of 7.5 MHz and Color Doppler wherever indicated.
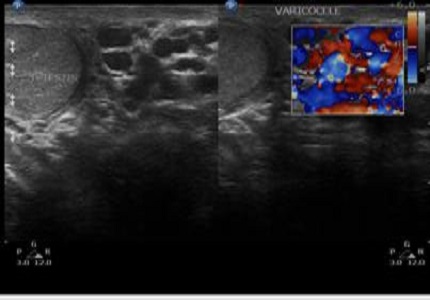
Results: Ultra sonographic findings of scrotum in 50 patients reveals 24 cases of varicocele, 7 cases of epididymal cysts, 8 cases of hydrocele, 3 cases of epididymitis, 2 cases of cryptorchidism, 2 cases of testicular microlithiasis and 1 case of bilateral testicular cyst. Apart from the patient who had cryptorchidism, the testis of all the patients were normal in size, site, shape and echo pattern. The clinical palpation when compared to ultrasound was found to be have a sensitivity of 58.33% and a specificity of 92.31%. The positive predictive value was found to be 87.50% and negative predictive value 70.59%.
Conclusion: Trans rectal and scrotal ultrasound provides valuable information in the diagnostic evaluation of infertile men and substantially more pathological conditions can be detected on ultrasound compared to clinical palpation.
Downloads
References
Ammar T, Sidhu PS, Wilkins CJ. Male infertility: the role of imaging in diagnosis and management. Br J Radiol. 2012 Nov;85 Spec No 1:S59-68. doi: https://doi.org/10.1259/bjr/31818161. Epub 2012 Jul 4.
Raza SA, Jhaveri KS. Imaging in male infertility. Radiol Clin North Am. 2012 Nov;50(6):1183-200. doi: https://doi.org/10.1016/j.rcl.2012.08.006.
Kumar N, Singh AK. Trends of male factor infertility, an important cause of infertility: A review of literature. J Hum Reprod Sci. 2015 Oct-Dec;8(4):191-6. doi: https://dx.doi.org/10.4103%2F0974-1208.170370.
Simpson WL Jr, Rausch DR. Imaging of male infertility: pictorial review. AJR Am J Roentgenol. 2009 Jun;192(6 Suppl):S98-107 (Quiz S108-11). doi: https://doi.org/10.2214/AJR.07.7109.
Brunereau L, Fauchier F, Fernandez P, Blais G, Royere G, Pourcelot L, Rouleau P, Tranquart F. [Sono graphic evaluation of human male in fertility]. J Radiol. 2000 Dec;81(12):1693-701.
Pethiyagoda AUB and Pethiyagoda K. Scrotal ultrasonography in the assessment of sub fertile males. International Journal of Scientific and Research Publications 2017;7(5):873-76.
Goullet E, Rigot JM, Blois N, Lemaitre L, Mazeman E. [Role of systematicscrotalultrasonography in the management of male infertility: prospective study of 609 cases]. Prog Urol. 2000 Feb;10(1):78-82.
Moon MH, Kim SH, Cho JY, Seo JT, Chun YK.ScrotalUS for evaluation of infertilemen with azoospermia. Radiology. 2006 Apr;239(1):168-73. Epub 2006 Feb 7.
Qublan HS, Al-Okoor K, Al-Ghoweri AS, Abu-Qamar A. Sonographic spectrum of scrotal abnormalities in infertile men. J Clin Ultrasound. 2007 Oct;35(8):437-41.
Eskew LA, Watson NE, Wolfman N, Bechtold R, Scharling E, Jarow JP. Ultra sonographic diagnosis of varicoceles. Fertil Steril. 1993 Oct;60(4):693-7.
Preutthipan S, Nicholas OA. Comparative study between scrotal physical examination and scrotal ultra sonography in the detection of varicocele in men with infertility. J Med Assoc Thai. 1995 Mar;78(3):135-9.
Gordon SJ, Otite U, Mahesh kumar P, Cannon P, Nargund VH. The use of scrotal ultrasonography in male infertility. BJU Int. 2001 Mar;87(4):417-8.
Jequier AM, Phillips N, Yovich JL. The Diagnostic Value of a Routine Genito-Urinary Ultrasound Examination for Men Attending an Infertility Clinic. Andrology & Gynecology: Current Research. 2014;2:4.
Ibrahim M, Tabari A, Igashi J, Lawal S, Ahmed M. Scrotal doppler ultrasound evaluation in Zaria, Nigeria. Nigerian Journal of Basic and Clinical Sciences. 2016;13(2):89.
Dogra VS, Gottlieb RH, Oka M, Rubens DJ.Sonography of the scrotum. Radiology. 2003 Apr;227(1):18-36. Epub 2003 Feb 28.
Ho KL, Tsu JH, Tam PC, Yiu MK. Disease spectrum and treatment patterns in alocalmale infertility clinic. Hong Kong Med J. 2015 Feb;21(1):5-9. doi: https://doi.org/10.12809/hkmj144376. Epub 2015 Jan 2.
Abdulwahed S, Mohamed E, Taha E, Saleh M, Abdelsalam Y, El Ganainy E. Sensitivity and Specificity of Ultra sonography in Predicting Etiology of Azoospermia. Urology. 2013;81(5):967-71.
Sakamoto H, Saito K, Shichizyo T, Ishikawa K, Igarashi A, Yoshida H. Color Doppler ultra sonography as a routine clinical examination in male infertility. Int J Urol. 2006 Aug;13(8):1073-8.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


