Blood stream infections with Candida species: a prospective study in a tertiary care center
Abstract
Aims and Objectives: To study the profile of blood stream infections with Candida species, their current epidemiological trend at our setting, clinical management, resistance trends and outcome in terms of mortality.
Methods: This is a prospective observational study conducted among all adult in-patients, at AIMS, Kochi from August 1st 2014 to February 28th 2016, both in wards and ICUs, who have positive isolates of Candida species in bloodstream infection among the positive blood culture samples. Incidence rate of Candidemia was calculated and distribution of Candidemia with respect to characteristics like age, gender, comorbid illness, mechanical ventilation, prior antibiotic therapy, prolonged ICU stay.
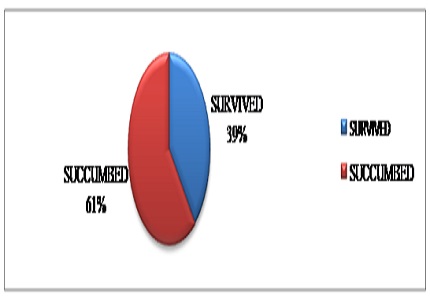
Results: Out of 1600 blood stream infection isolates, Candidemia was fourth most common blood stream isolate infection in our study with an incidence rate of 7.5%. Candida tropicalis was the predominant species in our study (30.8%). Mortality rate due to Candidemia was (61%). Urethral catheterization, Central venous access, neutropenia at presentation, prior antibiotic therapy, renal failure, Dialysis patients, prolonged ICU stay were some of the risk factors found to be statistically significant in assessing the mortality of patients in our study with a p value of <0.001.
Conclusion: All patients with Candidemia should be treated with an antifungal agent at the earliest without any delay, as delay causes increase in mortality. All vascular catheters should be removed to help clear Candida from blood more quickly. Improved survival was found with the use of an Echinocandin and the removal of central venous catheters.
Downloads
References
Gonzalez de Molina FJ, Leon C, Ruiz- Santana S et al (2012) Assessment of candidemia-attributable mortality in critically ill patients using propensity score matching analysis. Crit Care 16(3):R105 PMID:22698004 PMCID:PMC3580662. DOI: https://doi.org/10.1186/cc11388.
Bassetti M, Merelli M, Righi E et al. Epidemiology, species distribution, antifungal susceptibility, and outcome of candidemia across five sites in Italy and Spain. J ClinMicrobiol. 2013; 51(12):4167–4172. DOI: https://doi.org/10.1128/JCM.01998-13.
Playford EG, Marriott D, Nguyen Q et al. Candidemia in non-neutropenic critically ill patients: risk factors for non-albicans Candida spp. Crit Care Med.2008; 36(7):2034–2039 PMID:18552700. DOI: https://doi.org/10.1097/CCM.0b013e3181760f42.
Pappas PG, Rex JH, Lee J et al . A prospective observational study of candidemia: epidemiology, therapy, and influences on mortality in hospitalized adult and pediatric patients. Clin Infect Dis 2003;37(5):634–643 PMID:12942393 doi: https://doi.org/10.1086/376906.
Chen S, Slavin M, Nguyen Q et al. Active surveillance for candidemia, Australia. Emerg Infect Dis 2006; 12(10):1508–1516. doi: https://dx.doi.org/10.3201%2Feid1210.060389.
Leroy O, Mira JP, Montravers P et al (2010) Comparison of albicans vs. non-albicans candidemia in French intensive care units. Crit Care 14(3):R98.doi: https://doi.org/10.1186/cc9033.
Pfaller MA, Messer SA, Moet GJ et al (2011) Candida bloodstream infections: comparison of species distribution and resistance to echinocandin and azole antifungal agents in intensive care unit (ICU) and non-ICU settings in the SENTRY antimicrobial surveillance program (2008–2009). Int J Antimicrobial Agents 38(1):65–69 PMID:21514797. DOI: https://doi.org/10.1016/j.ijantimicag.2011.02.016.
Meyer E, Geffers C, Gastmeier P et al (2013) No increase in primary nosocomial candidemia in 682 German intensive care units during 2006–2011. Euro Surveill 18(24):20505PMID:23787164.
Chow JK, Golan Y, Ruthazer R et al (2008) Risk factors for albicans and non-albicans candidemia in the intensive care unit. Crit Care Med36 (7):1993–1998 PMID:18552702 DOI: https://doi.org/10.1097/CCM.0b013e31816fc4cd.
Leroy O, Gangneux JP, Montravers P et al (2009) Epidemiology, management, and risk factors for death of invasive Candida infections in critical care: a multicenter, prospective, observational study in France (2005–2006). Crit Care Med 37(5):1612–1618 1618 PMID:19325476 DOI: https://doi.org/10.1097/CCM.0b013e31819efac0.
Chakrabarti A, Chatterjee SS, Rao KL et al (2009) Recent experience with fungemia: change in species distribution and azole resistance. Scand J Infect Dis 41(4):275–284. PMID:19229762 DOI: https://doi.org/10.1080/00365540902777105.
Mootsikapun P, Hsueh PR, Talwar D et al (2013) Intravenous anidulafungin followed optionally by oral voriconazole for the treatment of candidemia in Asian patients: results from an open-label phase III trial. BMC Infect Dis 13:219.doi: https://doi.org/10.1186/1471-2334-13-219.
Blot SI, Vandewoude KH, Hoste EA et al (2002) Effects of Nosocomial Candidemia on outcomes of critically ill patients. Am J Med 113(6):480–485. PMID:12427497.
Kett DH, Azoulay E, Echeverria PM et al (2011) Candida bloodstream infections in intensive care units: analysis of the extended prevalence of infection in intensive care unit study. Crit Care Med 39(4):665–670. PMID:21169817 DOI: https://doi.org/10.1097/CCM.0b013e318206c1ca.
Leon C, Ostrosky-Zeichner L, Schuster M (2014) What’s new in the clinical and diagnostic manage- ment of Invasive Candidiasis in critically ill patients. PMID:24718642 DOI: https://doi.org/10.1007/s00134-014-3281-0.
Gudlaugsson O, Gillespie S, Lee K et al (2003) Attributable mortality of nosocomial candidemia, revisited. Clin Infect Dis 37(9):1172–1177. PMID:14557960 DOI: https://doi.org/10.1086/378745.
Fraser VJ, Jones M, Dunkel J, et al. Candidemia in a tertiary care hospital: epidemiology, risk factors, and predictors of mortality. Clin Infect Dis 1992; 15:414. PMID:1520786.
Quindos G. Epidemiology of candidaemia and invasive candidiasis. A changing face. Rev IberoamMicol. 2014;31:42-48. PMID:24270071 DOI: https://doi.org/10.1016/j.riam.2013.10.001.
Bitar D, Lortholary O, Le Strat Y, Nicolau J, Coignard B, Tattevin P, et al. Population based analysis of invasive fungal infections, France, 2001–2010. Emerg Infect Dis 2014;20:1149–55. PMID:24960557 PMCID:PMC4073874 DOI: https://dx.doi.org/10.3201%2Feid2007.140087.
Hidron AI, Edwards JR, Patel J, Horan T, Sievert DM, Pollock DA, et al. Antimicrobial-resistant pathogens associated with healthcare-associated infections: annual summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2006e2007. Infect Control HosplEpidemiol2008;29:996e1011. PMID:18947320 DOI: https://doi.org/10.1086/591861
Fridkin SK. The changing face of fungal infections in health care settings. Clin Infect Dis 2005; 41:1455.doi: https://doi.org/10.1086/497138
Wisplinghoff H, Bischoff T, Tallent SM, Seifert Wenzel RP, Edmond MB. Nosocomial bloodstream infections in US hospital: analysis of 24,179 cases from a prospective nationwide surveillance study. Clin Infect Dis 2004;39:309-17. doi: http://doi.org/10.1086/425328
Marchetti O, Bille J, Fluckinger U, Eggiman P, Ruef C, Garbino J, et al. Epidemiology of candidemia in Swiss tertiary care hospitals: secular trends, 1991–2000. Clin Infect Dis 2004;38:311–20.doi: http://doi.org/10.1086/380637
Gudlaugsson O, Gillespie S, Lee K, Vande Berg J, Hu J, Messer S, et al. Attributable mortality of nosocomial candidemia, revisited. Clin Infect Dis 2003;37:1172–7. PMID:14557960. DOI: https://doi.org/10.1086/378745.
Morgan J, Meltzer MI, Plikatys BD, Sofair AN, Huie-White S, Wilcox S, et al. Excess mortality, hospital stay and cost due to candidemia: a case–control study using data from population-based candidemia surveillance. Infect Control Hosp Epidemiol2005;26:540–7. PMID:16018429 DOI: https://doi.org/10.1086/502581
Liu CY, Liao CH, Chen YC, Chang SC. Changing epidemiology of nosocomial bloodstream infections in 11 teaching hospitals in Taiwan between 1993 and 2006. JMicrobiol, Immunol Infect 2010;43:416e29. . Journal of Microbiology, Immunology and Infection (2015) 48, 306 315.
Hobson RP. The global epidemiology of invasive Candida infections. Is the tide turning? J Hosp Infect 2003;55:159e68.PMID:14572481.
Ruan SY, Hsueh PR. Invasive Candidiasis overview: An overview from Taiwan. J Formos Med Assoc2009;108:443e51. PMID:19515624 DOI: https://doi.org/10.1016/S0929-6646(09)60091-7.
Horn DL, Neofytos D, Anaissie EJ, Fishman JA, Steinbach WJ, Olyaei AJ, et al. Epidemiology and outcomes of candidemia in 2019 patients: data from the prospective antifungal therapy alliance registry. Clin Infect Dis 2009;48:1695e703. PMID:19441981DOI: https://doi.org/10.1086/599039.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


