Histopathological and cytological spectrum of lymphadenopathy: a window to preliminary diagnosis
Abstract
Introduction: Lymphadenopathy is a common clinical presentation of patients attending outdoor patient departments. The etiology varies with a wide spectrum ranging from inflammatory causes on one end to malignant on the other. In the present study, cytological and relevant histopathological diagnoses were done in 200 cases received in Department of Pathology.
Aims and objectives: The present study aimed to find out the percentage of various lesions of lymph node and their prevalence according to age group and sex of patients. It also correlated the histo-cytodiagnosis in cases where both histology and cytology were available and compared the results of present study with similar other studies.
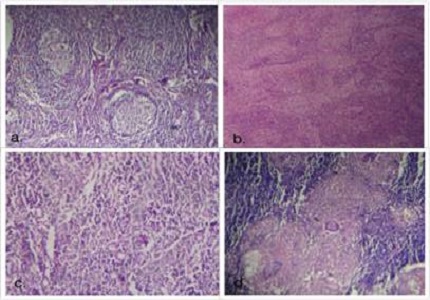
Materials and Methods: This study was carried out in the department of pathology, Govt. medical college, Patiala. It included 200 cases of lymphadenopathies, either from Rajindra hospital or from health centers nearby. The cases were selected randomly. Lymph nodes included were of neck region, axilla, groin, from the extremities and the internal (mediastinal, abdominal and retroperitoneal). Apart from haematoxylin and eosin (H & E) stain, special stains like Ziehl–Neelsen stain and giemsa stain were done wherever needed.
Results: Out of 200 cases, 93 (46.5%) cases were of reactive hyperplasia. Females were affected more commonly than males. Tuberculosis occurred more in younger patients whereas metastases were more common in older age group. Axillary lymph node was the most common lymph node involved.
Conclusion: Histopathology gave accurate and confirmatory results than cytology. Lymph node evaluation is an integral part of patient management.
Downloads
References
Delves PJ, Roitt IM. The immune system. First of two parts. N Engl J Med. 2000; 343:37-49. DOI: https://doi.org/10.1056/NEJM200007063430107.
Van der valk P, Meijer CJLM. Lymph nodes. In Mills SE: Histology for pathologists. 3rd ed. Philadelphia: Lippincott Williams and Wilkins; 2007; p. 763-82.
Cottier H, Turk J, Sobin L. A proposal for a standardized system of reporti ng human lymph node morphology in relation to immunological function. Bull World Health Organ. 1972; 47(3): 375-417.
Stein H, Bonk A, Tolksdor f G, Lennert K, Rodt H, Gerdes J. Immunohistologic analysis of the organization of normal lymphoid tissue and non-Hodgkin's lymphomas. J Histochem Cytochem. 1980 Aug;28(8):746-60.
Eroschenko VP. diFiore’s atlas of histology with functional correlations, 11th ed. New Delhi: Wolters Kluwer; 2009: 196-97.
Rosai J, Ackerman. Rosai and Ackerman’s Surgical Pathology. 9th ed. New Delhi: Elsevier; 2004; p.1772, 1879, 974.
Roitt IM. Essential immunology. 9th ed. London: Blackwell Publishing Company; 1997. Chapter 2, Specific acquired response; p.152-67.
Alice R, Bruce C. The lymphatic system. In Waldo Nelson, Behraman RE, Kleigman eds. Textbook of Pediatrics. 16th ed. Philadelphia: W.B. Saunders; p.1527-29.
Linet OI, Metzler C. Practical ENT. Incidence of palpable cervical nodes in adults. Postgrad Med. 1977 Oct;62(4):210-3.
Pangalis GA, Vassilakopoulos TP, Boussiotis VA, Fessas P. Clinical approach to lymphadenopathy. Semin Oncol. 1993 Dec;20(6):570-82.
Didlolker MS, Fanous N, Elias EG. Metastatic carcinomas from occult primary tumours. A study of 254 patients. Ann Surg. 1977; 186: 628-30.
Haagensen CD, Feind CR, Herter FP, Slanetz CA JR, Weinberg JA. The lymphatics in cancer. Philadelphia: W.B. Saunders; 1972.
Willis RA. The spread of tumours in the human body, 3rd ed. Stoneham: Butterworth; 1973.
Fijten GH, Blijham GH. Unexplained lymphadenopathy in family Practice-an evaluation of the probability of malignant causes and the effectiveness of physicians’ workup. J Fam Pract.1988 Oct; 27(4): 373-76.
Ferrer R. Lymphadenopathy: Differential diagnosis and Evaluation. American Family Physician. 1998 Oct 15; 58:1313-20.
Bazemore AW, Smucker DR. Lymphadenopathy and malignancy. American Family Physician. 2002 Dec 1; 66(11): 2103-10.
Ioachim HL, Medeiros LJ. Ioachim’s lymph node pathology, 4th ed. Philadelphia: Lippincott Williams and Wilkins; 2008.
Habermann TM, Steensma DP. Lymphadenopathy. Mayo Clin Proc. 2000 Jul;75(7):723-32.
Koss LG, Melamed MR. Diagnostic cytology and its histologic basis. 5th ed. Phildelphia: Lippincott Company; 2006.
Abdullah P, Mubarik A, Zahir N. The importance of lymph node biopsy in diagnosis of lymphadenopathy. J Coll Physicians Surg Pak 2000; 10(8): 298-301.
Dandapat MC, Mishra BM, Dash SP, Kar PK. Peripheral lymph node tuberculosis: a review of 80 cases. Br J Surg. 1990 Aug;77(8):911-2.
Shrestha AK, Chalise PR, Shrestha ML. Lymph node biopsies- A Hospital based retrospective study. J Nepal Med Assoc 2009; 48(176):306-9. PMCID: PMC3993046.
Lee B, Chang L. Fine Needle Aspiration Biopsy and Histopathologic Diagnosis in the Head and Neck Masses. Korean J Otolaryngol- Head Neck Surg. 1999 Nov; 42(11): 1429-34.
Zahir ST, Azimi A. Histopathologic findings of lymph node biopsy cases in comparison with clinical features. Pak J Med Sci. 2009; 25(5): 728-33. ISSN 1681-715X.
Thomas JO, Ladipo JK, Yawe T. Histopathology of lymphadenopathy in a tropical country. East Afr Med J. 1995 Nov;72(11):703-5.
Ojo BA, Buhari MO, Malami SA, Abdulrahaman MB. Surgical lymph node biopsies in University of Ilorin Teaching Hospital, Ilorin, Nigeria. Niger Postgrad Med J. 2005 Dec; 12(4): 299-304. PMID: 16380743.
Hirachand S, Lakhey M, Akhter J, Thapa B. Evaluation of fine needle aspiration cytology of lymph nodes in Kathmandu Medical College, Teaching hospital. Kathmandu Univ Med J (KUMJ). 2009 Apr-Jun;7(26):139-42.
Shaikh MS, Baloch I, Bhatti Y. An audit of 200 cases of cervical Lymphadenopathy. Medical Channel. 2010 Jan-Mar; 16: 85-7.
Olu-Eddo AN, Ohanaka CE. Peripheral lymphadenopathy in Nigerian adults. J Pak Med Assoc. 2006 sept; 56(9): 405-8. http://www.jpma.org.pk/PdfDownload/837.pdf
Bonadonna G. Historical review of Hodgkin’s disease. Br J Haematol. 2000; 110: 504-511. DOI: https://doi.org/10.1046/j.1365-2141.2000.02197.x.
Kardos TF, Vinson JH, Behm FG, Frable WJ, O'Dowd GJ. Hodgkin's disease: diagnosis by fine-needle aspiration biopsy. Analysis of cytologic criteria from a selected series. Am J Clin Pathol. 1986 Sep;86(3):286-91.
Jimenez-Heffernan JA, Vicandi, Lopez-Ferrer P. Value of the fine needle aspiration cytology in the initial diagnosis of Hodgkin’s disease: analysis of 188 cases with an emphasis on diagnostic pitfalls. Acta Cytol. 2001; 45(3): 300-06. PMID: 11393058.
Tani E, Ersoz C, Svedmyr E. Fine-needle aspiration cytology and immunocytochemistry of Hodgkin’s disease, suppurative type. Diagn cytopatho. 1998; 18(1): 1-4.
Iacobuzio-Donahue CA, Clark DP, Ali SZ. Reed-Sternberg-like cells in lymph node aspirates in the absence of Hodgkin’s disease: pathologic significance and differential diagnosis. Diagn Cytopatho. 2002 Dec; 27(6): 335-39.
Vezzoli P, Fiorani R, Girgenti V, Fanoni D, Tavecchio S, Balice Y, Mozzana R, Crosti C, Berti E. Cutaneous T-cell/histiocyte-rich B-cell lymphoma: a case report and review of the literature. Dermatology. 2011;222(3):225-30. doi: https://doi.org/10.1159/000327376. Epub 2011 Apr 30.
Volmar KE, Singh HK, Gong JZ. The advantages and limitations of the role of core needle and FNA biopsy of lymph nodes in the modern era: Hodgkin and non-Hodgkin Lymphomas and metastatic Disease. Pathology Case Reviews. 2007; 12(1): 10-26. DOI: https://doi.org/10.1097/01.pcr.0000252857.12872.52.
Dhingra V, Misra V , Mishra R , Bhatia R , Singhal M. Fine needle aspiration cytology as a diagnostic tool in pediatric lymphadenopathy. Journal of Clinical and Diagnostic Research 2010 June; 4: 2452-57.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


