Lung function tests in different phases of menstrual cycle
Abstract
Introduction: Menstrual cycle is an integral part of a woman’s life. During these different phases, rhythmic changes occur in the levels of ovarian hormones especially progesterone and estrogen. The goal of this study was to study the effect of the luteal and follicular phases of the menstrual cycle on bronchial reactivity (BR) in a group of women.
Material and Methods: The fifty girl medical students of first year MBBS of 18 – 24 years age were undertaken to study pulmonary function tests in different phases of menstrual cycle. Pulmonary function tests were taken between 8 – 10 th day of menstrual cycle, that is in follicular phase and again were recorded between 20 – 22 nd day of menstrual cycle that is in luteal phase by using spirometric technique. The results were expressed as Mean ± Standard Deviation (Mean+ SD). Statistical analysis was done through Graph pad prism. Comparison of pulmonary function parameters in different phases of menstrual cycle was done by using one way ANOVA (Analysis of Variance) by bonferroni post-hoc test.
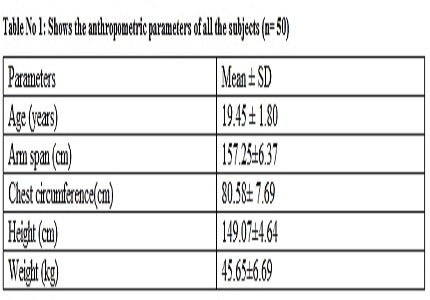
Results: Anthropometric measurement of all subjects in which mean age was 19.45 ± 1.80 years, arm span was 157.25± 6.37 cm, chest circumference was 80.58 ± 7.69 cm , height was 149.07 ±4.64 cm , weight was 45.65±6.69 Kgs. Spirometric study found FVC , FEV1, and PEFR increase in luteal phase of menstrual cycle compared to follicular phase, which were statistically significant.
Conclusion: We found better lung functions which were statistically significant in luteal phase as compared to follicular phase of our subjects indicating a possible role of progesterone causing β adrenergic stimulation / sensitization.
Downloads
References
Graziottin A, Zanello PP.[Menstruation, inflammation and comorbidities: implications for woman health]. Minerva Ginecol. 2015 Feb; 67(1):21-34. http://www.ncbi.nlm.nih.gov.
Graziottin A.The shorter, the better: A review of the evidence for a shorter contraceptive hormone-free interval..Eur J Contracept Reprod Health Care. 2016; 21(2):93-105. http://www.ncbi.nlm.nih.gov
Heitkemper MM, Cain KC, Jarrett ME, Burr RL, Hertig V, Bond EF.Symptoms across the menstrual cycle in women with irritable bowel syndrome. Am J Gastroenterol. 2003 Feb; 98(2):420-30. http://www.ncbi.nlm.nih.gov
Rubtsova K, Marrack P, Rubtsov AV. Sexual dimorphism in autoimmunity. J Clin Invest. 2015 Jun; 125(6):2187-93. http://www.ncbi.nlm.nih.gov
Zandman-Goddard G, Peeva E, Shoenfeld Y .Gender and autoimmunity. Autoimmun Rev. 2007 Jun; 6(6):366-72. http://www.ncbi.nlm.nih.gov
Graziottin A, Skaper SD, Fusco M. Inflammation and Chronic Pelvic Pain: A Biological Trigger for Depression in women? J Depress Anxiety. 2013;3:142–150. http://www.ncbi.nlm.nih.gov
Graziottin A, Skaper SD, Fusco M. Mast cells in chronic inflammation, pelvic pain and depression in women. Gynecol Endocrinol. 2014;30:472–7. doi: https://doi.org/10.3109/09513590.2014.911280.
Martin VT, Lipton RB. Epidemiology and biology of menstrual migraine. Headache. 2008;48(Suppl 3):S124–30. doi: https://doi.org/10.1111/j.1526-4610.2007.00947.x. http://www.ncbi.nlm.nih.gov
Hassan S, Muere A, Einstein G. Ovarian hormones and chronic pain: A comprehensive review. Pain. 2014;155:2448–60. doi: https://doi.org/10.1016/j.pain.2014.08.027. http://www.ncbi.nlm.nih.gov
Chandler MHH, Schuldheisz S, Phillips BA, Muse KN. Premenstrual asthma: the effect of estrogen on symptoms, pulmonary function, and β2-receptors. Pharmacotherapy. 1997;17:224–234. http://www.ncbi.nlm.nih.gov
Agrawal AK, Shah A. Menstrual-linked asthma. J Asthma. 1997;34:539–545. http://www.ncbi.nlm.nih.gov
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, Enright P, van der Grinten CP, Gustafsson P, Jensen R, Johnson DC, MacIntyre N, McKay R, Navajas D, Pedersen OF, Pellegrino R, Viegi G, Wanger J. J; ATS/ERS Task Force. Standardisation of Spirometry. Eur Resp J. 2005;26:319–338. http://www.ncbi.nlm.nih.gov
Berbic M, Fraser IS. Immunology of normal and abnormal menstruation. Womens Health (Lond Engl) 2013;9:387–95. doi: https://doi.org/10.2217%2FWHE.13.32. http://www.ncbi.nlm.nih.gov
Lockwood CJ. Mechanisms of normal and abnormal endometrial bleeding. Menopause. 2011;18:408–11. doi: https://dx.doi.org/10.1097%2FGME.0b013e31820bf288. http://www.ncbi.nlm.nih.gov
Berbic M, Ng CH, Fraser IS. Inflammation and endometrial bleeding. Climacteric. 2014;23:1–7. http://www.ncbi.nlm.nih.gov
Menzies FM, Shepherd MC, Nibbs RJ, Nelson SM. The role of mast cells and their mediators in reproduction8 pregnancy and labour. Hum Reprod Update. 2011;17:383–96. doi: https://doi.org/10.1093/humupd/dmq053. http://www.ncbi.nlm.nih.gov
Muñoz-Cruz S, Mendoza-Rodríguez Y, Nava-Castro KE, Yepez-Mulia L, Morales-Montor J. Gender-Related Effects of Sex Steroids on Histamine Release and FcεRI Expression in Rat Peritoneal Mast Cells. J Immunol Res. 2015;2015:351829. doi: https://doi.org/10.1155/2015/351829.
Kim MS1, Chae HJ, Shin TY, Kim HM, Kim HR. Estrogen regulates cytokine release in human mast cells. Immunopharmacol Immunotoxicol. 2001;23:495–504. doi: https://doi.org/10.1081/IPH-100108596.
Vasiadi M, Kempuraj D, Boucher W, Kalogeromitros D, Theoharides TC. Progesterone inhibits mast cell secretion. Int J Immunopathol Pharmacol. 2006;19:787–94. http://www.ncbi.nlm.nih.gov
Osman M. Therapeutic implications of sex differences in asthma and atopy. Arch Dis Child. 2003;88:587–90. doi: http://dx.doi.org/10.1136/adc.88.7.587. http://www.ncbi.nlm.nih.gov
Zhao XJ, McKerr G, Dong Z, Higgins CA, Carson J, Yang ZQ, et al. Expression of oestrogen and progesterone receptors by mast cells alone, but not lymphocytes, macrophages or other immune cells in human upper airways. Thorax. 2001;56:205–11. doi: http://dx.doi.org/10.1136/thorax.56.3.205. http://www.ncbi.nlm.nih.gov
Alessandra Graziottin et al Perimenstrual asthma: from pathophysiology to treatment strategies. Multidiscip Respir Med. 2016; 11: 30. Published online 2016 Aug 1. doi: https://doi.org/10.1186/s40248-016-0065-0. http://www.ncbi.nlm.nih.gov
Dratva J1, Schindler CPerimenstrual increase in bronchial hyperreactivity in premenopausal women: results from the population-based SAPALDIA 2 cohort. J Allergy Clin Immunol. 2010 Apr;125(4):823-9. http://www.ncbi.nlm.nih.gov
Venkatachalem Sathish Sex Steroid Signaling: Implications for Lung Diseases. Pharmacol Ther. 2015 Jun; 150: 94–108. http://www.ncbi.nlm.nih.gov
Elizabeth A. Townsend Sex Differences and Sex Steroids in Lung Health and Disease. Endocr Rev. 2012 Feb; 33(1): 1–47. Published online 2012 Jan 12. http://www.ncbi.nlm.nih.gov
Pugh ME, Hemnes A. Development of pulmonary arterial hypertension in women: interplay of sex hormones and pulmonary vascular disease. Womens Health (Lond). 2010 Mar; 6(2):285-96. http://www.ncbi.nlm.nih.gov
Sakao S, Tanabe N, Tatsumi K. The estrogen paradox in pulmonary arterial hypertension. Am J Physiol Lung Cell Mol Physiol. 2010 Oct; 299(4):L435-8. http://www.ncbi.nlm.nih.gov
Tofovic SP. Estrogens and development of pulmonary hypertension: interaction of estradiol metabolism and pulmonary vascular disease. J Cardiovasc Pharmacol. 2010 Dec; 56(6):696-708. http://www.ncbi.nlm.nih.gov
Lahm T, Crisostomo PR, Markel TA, Wang M, Weil BR, Novotny NM, Meldrum DR. The effects of estrogen on pulmonary artery vasoreactivity and hypoxic pulmonary vasoconstriction: potential new clinical implications for an old hormone. Crit Care Med. 2008 Jul; 36(7):2174-83. http://www.ncbi.nlm.nih.gov.
Smith AM, Bennett RT, Jones TH, Cowen ME, Channer KS, Jones RD. Characterization of the vasodilatory action of testosterone in the human pulmonary circulation. Vasc Health Risk Manag. 2008; 4(6):1459-66. http://www.ncbi.nlm.nih.gov.
Fuseini H Mechanisms Driving Gender Differences in Asthma. Curr Allergy Asthma Rep. 2017 Mar;17(3):19. http://www.ncbi.nlm.nih.gov.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


