Interstitial lung diseases - a tertiary care center experience
Abstract
Introduction: Interstitial lung diseases are a group of diffuse parenchymal lung disorders associated with substantial morbidity and mortality and pose diagnostic and therapeutic challenges to the clinician. Diagnosis of ILD is by multidisciplinary discussion (MDD) between clinician, radiologist and pathologist. The incidence and prevalence of ILDs in India are unknown. Prospective disease registries can provide better estimates of incidence and prevalence as well as insights to etiology, associated risks, natural history, and outcomes of a disease. This was a prospective study undertaken to analyse the spectrum of ILD encountered, demographic profile, clinical and radiological characteristics of the patients with interstitial lung disease in a tertiary care setting.
Materials and Methods: A prospective study over a period of two years conducted at Medical College,Thiruvananthapuram. 164 consecutive patients with multidisciplinary diagnosis of interstitial lung disease were included in the study. Detailed history, spirometry, SPO2, DLCO, HRCT, 6 minute walk test,ECG,2D ECHO were done and recorded in duly filled proforma. ANA profile, serum angiotensin converting enzyme,serum calcium, 24 hour urinary calcium were estimated wherever it was indicated. Diagnosis of IPF was done after excluding the known causes and the HRCT findings suggestive of UIP pattern based on the current guidelines of the American Thoracic Society/European Respiratory Society 2013.
Statitical Analysis: Data were entered in Microsoft Excel and analyzed using Epi Info version 7. For descriptive statistics, quantitative variables were described by mean and standard deviation. Qualitative variables were described by percentage distribution. For inferential statistics between groups, comparison of qualitative variables were analysed by chi-square test and quantitative variables were compared by student t test. P value of less than 0.05 was considered as level of significance.
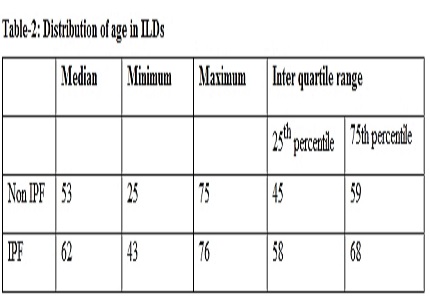
Result: 164 consecutive ILD patients were included in the study.Of this 26.26% patients were IPF and 73.74% were non-IPF. CTD-ILD was the most common (64%). Mean age of the study population was 54.03 ± 11.08 years. The mean age was higher among IPF patients (61.41±7.7) compared to non-IPF ILD patients (51.4±10.9). 65.8% of study populations were were females. Among IPF patients, 65.1% were males (95%CI: 49.07%, 78.99%) compared to 23.2% (95% CI: 15.96%, 31.68%) males in non- IPF group (p< .001). The proportion of ever smokers was higher among IPF patients (62.7%), 95% CI: 46.7%, 77.02%) compared to non IPF group (15.7%), 95% CI: 9.7%, 23.43%) (p <.001) . IPF patients had lower mean FVC % compared to non- IPF ILDs.(48.1±16.2 vs 51.2±23.8)(p<.001). The mean DLCO was lower among IPF patients (42.6±9.92 vs 53.9±15.22) compared to non-IPF group at presentation (p<.002). The mean 6MWD was lower among IPF patients (209.6±96.30 meters compared to non-IPF (288.6±101.2) meters (P<.001). IPF patients had lower mean SpO2 (90.13±3.5) compared to non-IPF group (93.82±2.86). 100% of IPF patients had UIP pattern in HRCT where as, 9.92%, of patients (95% CI: 5.2%, 16.6%) among non-IPF group had UIP pattern in HRCT (p<.001). In IPF patients, the proportion of patients with pulmonary HTN was higher (53.49%, 95% CI: 37.65%, 68.82%) compared to non-IPF (21.49%, 95% CI: 14.5%, 29.8%). GERD symptoms were more common among IPF patients (74.4%) compared to 67.7% among non IPF,which was not statistically significant. (p 0.41).
Conclusion: Out of 164 ILD patients, 26.2% were IPF. Among non –IPF group, CTD-ILD was the commonest. The mean age was higher among IPF patients, compared to non-IPF ( p value = 0.001.)IPF was more common in males, where as females predominate in Non-IPF group (p<0.001) The proportion of ever smokers was higher among IPF patients (62.7%). FVC%, DLCO%, 6MWD, SPO2 were lower in IPF compared to non –IPF, at the time of presentation(p< 0.001). HRCT showed UIP pattern in 100% of IPF. Proportion of patients with pulmonary HTN was higher in IPF (53.49%,) compared to non-IPF (21.49%,). GERD symptoms were present in 69.5% of study population.
Downloads
References
KaterinaM. Antoniou, George,A. Margaritopoulos, Sara Tomassetti. Interstitial lung disease. European Respiratory Review 2014 23: 40-54.
William D. Travis, Ulrich Costabel, David M. Hansell, Talmadge E. King, Jr., David A. Lynch, Andrew G. An Official American Thoracic Society/European Respiratory Society Statement: Update of the International Multidisciplinary Classification of the Idiopathic Interstitial Pneumonias 2013.
Ganesh Raghu and Sanjeev Mehta. Interstitial lung disease (ILD) in India: Insights and lessons from the prospective, landmark ILD-India registry. Lung India. 2016 Nov-Dec; 33(6): 589–591.
Kumar Adesh, Yadav Prashant, Gupta K. Ashish, Gautam K. Aditya, Kumar Anand. Profile of interistial lung diseases at tertiary care centre of northern India. European journal of pharmaceuticaland medical research, 2016,3(8), 368-374.
Kumar R, Gupta N, Goel N. Spectrum of interstitial lung disease at a tertiary care centre in India. Pneumonol Alergol Pol. 2014;82(3):218-26. doi: 10.5603/PiAP.2014.0029.
Somenath Kundu, Subhra Mitra, Joydeep Ganguly, Subhasis Mukherjee ,Souvik Ray Ritabrata Mitra. Spectrum of diffuse parenchymal lung diseases with special reference to idiopathic pulmonary fibrosis and connective tissue disease: An eastern India experience. Lung India 2014;31:354-60.
Garin MC, Highland KB, Silver RM, Strange C. Limitations to the 6-minute walk test in interstitial lung disease and pulmonary hypertension in scleroderma. J Rheumatol. 2009 Feb;36(2):330-6. doi: https://doi.org/10.3899/jrheum.080447. Epub 2009 Jan 22.
Smith JS, Gorbett D, Mueller J, Perez R, Daniels CJ. Pulmonary hypertension and idiopathic pulmonary fibrosis: a dastardly duo.Am J Med Sci. 2013;346(3):221-5.
Sheetu Singh Bridget F. Collins , Bharat B. Sharma Jyotsna M. Joshi. Interstitial Lung Disease in India. Results of a Prospective Registry. American Journal of Respiratory and Critical Care MedicineVol. 195, No. 6 , 2017.
The ILD India Registry: A Novel Tool for Epidemiological Surveillance of Interstitial Lung Disease in India. Indian J Chest Dis Allied Sci 2013;55:197-199.
Singh V, Sharma BB. Laying the ground for research of interstitial lung disease in our country: ILD India registry. Lung India. 2014 Oct;31(4):320-2. doi: https://dx.doi.org/10.4103%2F0970-2113.142091.
Kumar R, Gupta N, Goel N. Spectrum of interstitial lung disease at a tertiary care centre in India. Pneumonol Alergol Pol. 2014;82(3):218-26. doi: https://doi.org/10.5603/PiAP.2014.0029.
Khantal N, Dubey A. Profile of Idiopathic Pulmonary Fibrosis cases at a tertiary care Institute. Int J Med Res Rev2015;3(7):717-720. doi: 10.17511/ijmrr.2015.i7.135.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


