Prognostic value of P53 nuclear overexpression in bladder cancer
Abstract
Introduction: Urinary bladder cancer is one of the common genitourinary malignancy presenting to the urology department. Prognosis of these patients will depend upon the number of clinicopathological factors. Overexpression of p53 is associated with aggressive behaviour of bladder cancer. The purpose of the present study is to assess the role of p53 tumour suppressor gene as an independent prognostic marker.
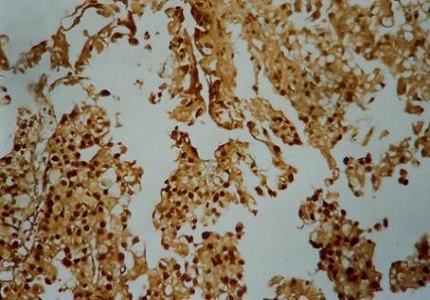
Materials & Methods: Thirty-three (33) consecutive cases of urinary bladder cancer attending Department of Urology between August 2006 to December 2008 were studied. In this study P53 protein, nuclear over expression was assessed in Formalin-fixed, paraffin-embedded tissue sections by the immunohistochemical method using monoclonal antibody. This p53 nuclear over expression was correlated with tumour grade and stage. Over all survival rate was assessed in p53 positive and negative patients.
Results: Two patients with T1G1 tumours developed recurrence with initial TURBT and intravesical BCG instillation after 6 months and responded to Re TURBT and intravesical BCG instillation therapy. One patient of T1G3 developed recurrence after 1 year with initial TURBT and intravesical BCG instillation and responded to Re TURBT and intravesical BCG instillation therapy. One patient of T1G3 progressed to muscle invasive disease after 1 year and underwent Radical cystoprostatectomy with ileal conduit received adjuvant chemotherapy and radiotherapy. Two patients developed post-operative urinary leak and underwent bilateral cutaneous ureterostomy. Nine patients died in followup period.
Conclusion: There was a strong positive correlation between the expression of mutant p53 and tumour grade, with none of the low-grade tumours were positive for mutant p53, in contrast to 60% of high-grade tumours. In this study, there was no significant difference in the mortality between p53 positive and negative patients.
Downloads
References
Jemal A, Murray T, Ward E, Samuels A, Tiwari RC, Ghafoor A, Feuer EJ, Thun MJ. Cancer statistics, 2005. CA Cancer J Clin. 2005 Jan-Feb;55(1):10-30.
Linn JF, Sesterhenn I, Mostofi FK, Schoenberg M. The molecular characteristics of bladder cancer in young patients. J Urol. 1998 May;159(5):1493-6.
Crow P, Ritchie AW. National and international variation in the registration of bladder cancer. BJU Int. 2003 Oct;92(6):563-6.
Harris CC, Hollstein M. Clinical implications of the p53 tumor-suppressor gene. N Engl J Med. 1993 Oct 28;329(18):1318-27.
Vogelstein B. Cancer. A deadly inheritance. Nature. 1990 Dec 20-27;348(6303):681-2.
Cote RJ, Chatterjee SJ. Molecular determinants of outcome in bladder cancer. Cancer J Sci Am. 1999 Jan-Feb;5(1):2-15.
Lozano G, Elledge SJ. p53 sends nucleotides to repair DNA. Nature. 2000 Mar 2;404(6773):24-5.
Smith ML, Chen IT, Zhan Q, Bae I, Chen CY, Gilmer TM, Kastan MB, O'Connor PM, Fornace AJ Jr. Interaction of the p53-regulated protein Gadd45 with proliferating cell nuclear antigen. Science. 1994 Nov 25;266(5189):1376-80.
Grossfeld GD, Ginsberg DA, Stein JP, et al: Thrombospondin-1 expression in bladder cancer: Association with p53 alterations, tumour angiogenesis, and tumour progression. J Natl Cancer Inst 1997; 89:219-27.
Carr AM. Cell cycle. Piecing together the p53 puzzle. Science. 2000 Mar 10;287(5459):1765-6.
Finlay CA, Hinds PW, Tan TH, Eliyahu D, Oren M, Levine AJ. Activating mutations for transformation by p53 produce a gene product that forms an hsc70-p53 complex with an altered half-life. Mol Cell Biol. 1988 Feb;8(2):531-9.
Messing EM, Reznikoff CA. Normal and malignant human urothelium: in vitro effects of epidermal growth factor. Cancer Res. 1987 May 1;47(9):2230-5.
Neal DE, Sharples L, Smith K, et al: The epidermal growth factor receptor and the prognosis of bladder cancer. Cancer 1990; 65:1619-25.
Popov Z, Gil-Diez-De-Medina S, Ravery V, et al: Prognostic value of EGF receptor and tumor cell proliferation in bladder cancer: Therapeutic implications. Urol Oncol 2004; 22:93-101.
Roberts AB, Sporn MB. Physiological actions and clinical applications of transforming growth factor-beta (TGF-beta). Growth Factors. 1993;8(1):1-9.
Coombs LM, Pigott DA, Eydman DA, et al: Reduced expression of TGFβ is associated with advanced disease in transitional cell carcinoma. Br J Cancer 1993; 67(3):578-584.
Esrig D, Elmajian D, Groshen S, Freeman JA, Stein JP, Chen SC, Nichols PW, Skinner DG, Jones PA, Cote RJ. Accumulation of nuclear p53 and tumor progression in bladder cancer. N Engl J Med. 1994 Nov 10;331(19):1259-64.
Gardner RA, Walsh MD, Allen V, et al: Immunohistological expression of p53 in primary pT1 transitional cell bladder cancer in relation to tumor progression. Br J Urol 1994; 73:526-32.
Lebret T, Becette V, Barbagelatta M, et al: Correlation between p53 overexpression and response to bacillus Calmette-Guérin therapy in a high risk select population of patients with pT1G3 bladder cancer. J Urol 1998; 159:788-91.
Lipponen PK. Over-expression of p53 nuclear oncoprotein in transitional-cell bladder cancer and its pro gnostic value. Int J Cancer. 1993 Feb 1;53(3):365-70.
Cordon-Cardo C: Mutation of cell cycle regulators—biological and clinical implications for human neoplasia. Am J Pathol 1995; 147(3):545-60.
Olumni AF, Tsai YC, Nichols PW, et al: Allelic loss of chromosome 17p distinguishes high grade from low grade transitional cell carcinomas of the bladder. Cancer Res 1990; 50:7081-3.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


