Clinicobacterial and histopathological study of chronic dacryocystitis
Abstract
Introduction: Diseases of lacrimal drainage system account for nearly 3% of visits to eye clinic. Chronic dacryocystitis is a frequently encountered disorder among these patients. The aim of this study was to identify the organisms responsible and to determine the antibiotic susceptibility pattern of the bacterial isolates from conjunctiva and nasal mucosa in cases of chronic dacryocystitis and comparing with lacrimal sac specimen.
Material and Methods: Prospective longitudinal study carried out in 40 cases suffering from chronic dacryocystitis. After complete history and local examination of the cases, the sac was excised and examined histopathologically in pathology department. Swabs of the smear were taken in all cases were cultured and antibiotic sensitivity was done. The results were analyzed by using mean, median and the Chi-square (χ2) test.
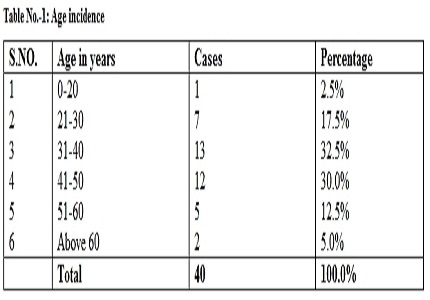
Results: The maximum incidence of the disease has been in the 4th and 5th decade of life, females were more predominantly affected than the males. The epithelial hypertrophy was the most common histological finding i.e 77.5%, the second common was squamous metaplasia followed by goblet cell formation. Culture and antibiotic sensitivity was done in all cases; out of these the maximum cases were found to be sterile i.e.55%. The bacteria which have been isolated in the 45% cases in order of frequency were staphylococcus 20%, streptococcus12.5% and pneumococcus 12.5% respectively.
Conclusion: Majority of the chronic dacryocystitis cases are caused by Staphylococcus, streptococcus and pneumococcus. Amoxyclav and 3rd generation cephalosporins can be used to treat chronic dacryocystitis. The epithelial hypertrophy and Non-specific chronic inflammation with fibrosis is indeed the most commonly reported histopathological finding in lacrimal sac wall biopsy specimens. Microbiological analysis and antimicrobial susceptibility pattern is mandatory for the selection of a specific antimicrobial therapy and to the control of further resistance development of bacterial strains.
Downloads
References
Gupta AK, Raina UK, Gupta A. The Lacrimal Apparatus. In: Text Book of Opthalmology. 1st edn. New Delhi, BI Churchill Livingstone 1999; 275–77.
Nayak N. Fungal infections of the eye--laboratory diagnosis and treatment. Nepal Med Coll J. 2008 Mar;10(1):48-63.
Chaudhary M, Bhattarai A, Adhikari SK, Bhatta DR. Bacteriology and antimicrobial susceptibility of adult chronic dacryocystitis. Nepal J Ophthalmol. 2010 Jul-Dec;2(2):105-13. doi: https://doi.org/10.3126/nepjoph.v2i2.3716.
Bartley GB. Acquired lacrimal drainage obstruction: an etiologic classification system, case reports, and a review of the literature. Part 1. Ophthal Plast Reconstr Surg. 2003;8(4):237–242.
Hartikainen J, Lehtonen OP, Saari KM. Bacteriology of lacrimal duct obstruction in adults. Br J Ophthalmol. 2009;81(1):37–40.
Das JK, Deka AC, Kuri GC, Bhattacharjee K, Das D, Gogoi K. Bacteriology of chronic dacryocystitis in adult population of northeast India. Orbit. 2008;27(4):243-7. doi: 10.1080/01676830802224668.
Chaudhary M, Bhattarai A, Adhikari SK. Bacteriology and antimicrobial susceptibility of adult chronic dacryocystitis. Nep J Oph. 2010;2(4):105–113.
Walland MJ, Rose GE. Soft tissue infections after open lacrimal surgery. Ophthalmol. 2011;101(3):608–11.
Collee JG, Miles RS, Watt B. Tests for the identification of bacteria. In:Collee JG, Fraser AG, Marmion BP, Simmons A. Mackie and McCartney, Practical Medical Microbiology, 14th ed. New Delhi: Elsevier, 2006; 13149.
Matthew AW, Franklin RC, William AC, Michael ND, George ME, David WH, et al. Performance Standards for Antimicrobial Susceptibility Testing; Fifteenth Informational supplement. 2005; 25(1):19-33. http://www.jcdr.net/article
Mandal R, Banerjee AR, Biswas MC, Mondal A, Kundu PK, Sasmal NK. Clinicobacteriological study of chronic dacryocystitis in adults. J Indian Med Assoc. 2008 May;106(5):296-8.
Ali MJ, Joshi SD, Naik MN, Honavar SG. Clinical profile and management outcome of acute dacryocystitis: two decades of experience in a tertiary eye care center. 2013.
Ali MJ, Motukupally SR, Joshi SD, Naik MN. The microbiological profile of lacrimal abscess: two decades of experience from a tertiary eye care center. J Ophthalmic Inflamm Infect. 2013 Jul 27;3(1):57. doi: https://doi.org/10.1186/1869-5760-3-57.
Kikkawa DO, Heinz GW, Martin RT, Nunery WN, Eiseman AS. Orbital cellulitis and abscess secondary to dacryocystitis. Arch Ophthalmol. 2002 Aug;120(8):1096-9.
Maheshwari R, Maheshwari S, Shah T. Acute dacryocystitis causing orbital cellulitis and abscess. Orbit. 2009;28(2-3):196-9.
Schmitt NJ, Beatty RL, Kennerdell JS. Superior ophthalmic vein thrombosis in a patient with dacryocystitis induced orbital cellulitis. Ophthal Plast Reconstr Surg. 2005;3:387–389. doi: https://doi.org/10.1097/01.iop.0000176269.84949.96.
Chaudhry IA, Shamsi FA, Al-Rashed W. Bacteriology of chronic dacryocystitis in a tertiary eye care center. Ophthal Plast Reconstr Surg. 2005 May;21(3):207-10.
Das JK, Deka AC, Kuri GC, Bhattacharjee K, Das D, Gogoi K. Bacteriology of chronic dacryocystitis in adult population of northeast India. Orbit. 2008;27(4):243-7. doi: 10.1080/01676830802224668.
Kebede A, Adamu Y, Bejiga A. Bacteriological study of dacryocystitis among patients attending in Menelik II hospital, Addis Ababa, Ethiopia. Ethiop Med J. 2010;3:29–33.
Briscoe D, Rubowitz A, Assia E. Changing bacterial isolates and antibiotic sensitivities of purulent dacryocystitis. Orbit. 2005;3:95–98. doi: https://doi.org/10.1080/01676830590926585.
Mills DM, Bodman MG, Meyer DR, Morton AD 3rd. The microbiologic spectrum of acute dacryocystitis. A national study of acute versus chronic infection. Ophthal Plast Reconstr Surg. 2007;3:302–306. doi: 10.1097/IOP.0b013e318070d237.
Razavi ME, Ansari-Astaneh MR, Farzadnia M, Rahmaniyan H, Moghiman T. Bacteriological evaluation of adult dacryocystitis in Iran. Orbit. 2010 Oct;29(5):286-90. doi: https://doi.org/10.3109/01676831003664293. Epub 2010 Aug 16.
Sun X, Liang Q, Luo S, Wang Z, Li R, Jin X. Microbiological analysis of chronic dacryocystitis. Ophthalmic Physiol Opt. 2005;3:261–263. doi: https://doi.org/10.1111/j.1475-1313.2005.00284.x.
Mohammad Javed Ali, 1 Swapna R Motukupally, The microbiological profile of lacrimal abscess: two decades of experience from a tertiary eye care center J Ophthalmic Inflamm Infect. 2013; 3: 57.
Relhan N1, Albini TA1, Pathengay A Endophthalmitis caused by Gram-positive organisms with reduced vancomycin susceptibility: literature review and options for treatment. Br J Ophthalmol. 2016 Apr;100(4):446-52. doi: http://dx.doi.org/10.1136/bjophthalmol-2015-307722. Epub 2015 Dec 23.
Assefa Y1, Moges F et al Bacteriological profile and drug susceptibility patterns in dacryocystitis patients attending Gondar University Teaching Hospital, Northwest Ethiopia. BMC Ophthalmol. 2015 Apr 2;15:34. doi: https://doi.org/10.1186/s12886-015-0016-0.
Teweldemedhin M1,2, Saravanan M Ocular bacterial infections at Quiha Ophthalmic Hospital, Northern Ethiopia: an evaluation according to the risk factors and the antimicrobial susceptibility of bacterial isolates. BMC Infect Dis. 2017 Mar 14;17(1):207. doi: https://doi.org/10.1186/s12879-017-2304-1.
Bernardini FP1, Moin M, Routine histopathologic evaluation of the lacrimal sac during dacryocystorhinostomy: how useful is it? Ophthalmology. 2002 Jul;109(7):1214-7; discussion 1217-8.
Alkatan H1, Al-Qurashi M Is routine histopathological examination of dacryocystorhinostomy/dacryocystectomy specimens necessary? A tertiary eye hospital experience. Can J Ophthalmol. 2017 Feb;52(1):34-41. doi: https://doi.org/10.1016/j.jcjo.2016.08.004. Epub 2016 Nov 17.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


