Antimicrobial resistance pattern of faecal Escherichia coli isolates: story of antibiotic use and misuse
Abstract
Introduction: Antimicrobial resistance is a major challenge of concern for treating patients. Emergence of antibiotic resistance among hospitalized patients has received considerable emphasis, while multi drug resistance also has an impact on community. It is well known that commensal faecal flora are reservoir of resistance genes, as well as site where resistance genes can be transferred.
Aims & Objectives: The aim of the present study was to determine the antimicrobial resistance pattern of Escherichia coli isolates from patients with suspected intestinal infection with and without diarrhoea attending outpatient department in tertiary care center.
Material & Methods: This retrospective short observational study was carried out on 111 non repetitive fecal samples received in microbiology laboratory. Escherichia coli (E.coli) strains isolated were evaluated for resistance pattern.
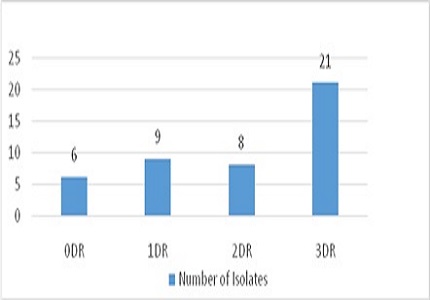
Results: Among 46(41.81%) isolated E.coli strains 84.78% isolates exhibited resistance to two or more antimicrobials, whereas 45.65% isolates were multi drug resistant. Decreased susceptibility was observed for first line antibiotics which tend to be more affordable and accessible to families, followed by 3rd generation cephalosporin’s. However, resistance among quinolones and aminoglycosides varies between 20-30%. Imipenem was observed as most sensitive followed by Piperacillin + Tazobactum (100.00% and 86.95% respectively).
Conclusion: Consequences of resistance are harder to define than microbiologists might wish. Some patients recover despite inadequate treatment whereas others failed to respond despite appropriate therapy. Increased morbidity and mortality are the most dramatic consequences of drug resistance.
Downloads
References
Calva JJ, Osorino JS, Ceron C. Antimicrobial resistance in fecal flora: longitudinal community based surveillance of children from urban Mexico. Antimicrobial agents & chemotherapy. 1996 Jul;40(7):1699-1702.
Livermore DM. Bacterial resistance: origins, epidemiology, and impact. Clin Infect Dis. 2003 Jan 15;36(Suppl 1):S11-23.
Bridges BA. Hypermutation in bacteria and other cellular systems. Philos Trans R Soc Lond B Biol Sci. 2001 Jan 29;356(1405):29-39.
Poole K. Multidrug efflux pumps and antimicrobial resistance in Pseudomonas aeruginosa and related organisms. J Mol Microbiol Biotechnol. 2001 Apr;3(2):255-64.
Cohen SP, McMurry LM, Hooper DC, Wolfson JS, Levy SB. Cross-resistance to fluoroquinolones in multiple-antibiotic–resistant (Mar) Escherichia coli selected by tetracycline or chloramphenicol: decreased drug accumulation associated with membrane changes in addition to OmpF reduction. Antimicrob Agents Chemother 1989 Aug;33(8):1318–25.
Livermore DM. Antibiotic resistance in staphylococci. Int J Antimicrob Agents. 2000 Nov;16 Suppl 1:S3-10.
Hall RM. Mobile gene cassettes and integrons: moving antibiotic resistance genes in gram-negative bacteria. Ciba Found Symp. 1997;207:192-202; discussion 202-5.
Bauernfeind A, Chong Y, Lee K. Plasmid-encoded AmpC beta-lactamases: how far have we gone 10 years after the discovery? Yonsei Med J. 1998 Dec;39(6):520-5.
Oliver A, Perez-Diaz JC, Coque TM, Baquero F, Canton R. Nucleotide sequence and characterization of a novel cefotaxime-hydrolyzing b-lactamase.(CTX M-10) isolated in Spain. Antimicrob Agents Chemother 2001Feb;45(2):616–20. DOI: https://doi.org/10.1128/AAC.45.2.616-620.2001.
Livermore DM. beta-Lactamases in laboratory and clinical resistance. Clin Microbiol Rev. 1995 Oct;8(4):557-84.
Carlet J. The gut is epicenter of antibiotic resistance. Antimicrobial resistance and infection control. 2012 Nov;1:39. DOI: https://doi.org/10.1186/2047-2994-1-39.
Rasheed MU, Thajuddin N, Ahamed P, Teklemariam Z, Jamil K. Antimicrobial drug resistance in strains of Escherichia coli isolated from food sources. Rev Inst Med Trop Sao Paulo. 2014 Jul-Aug;56(4):341-6.
Murray BE. Problems and dilemmas of antimicrobial resistance. Pharmacotherapy. 1992;12(6 Pt 2):86S-93S.
Collee JG, Duguid JP, Fraser AG, Marmion B P, Simmons A. Laboratory strategy in the diagnosis of infective syndrome. In Collee JG, Fraser AG, Marmion BP, Simmons A, editors. Mackie & McCartney Practical Medical Microbiology. 14thed. New Delhi: Elsevier, a division of Reed Elsevier India Pvt. Ltd. 2006. P.53-94.
Katouli M. Population structure of gut Escherichia coli and its role in development of extra-intestinal infections. Iran J Microbiol. 2010 Jun;2(2):59-72.
Aly MEA, Essam TM, Amin MA. Antibiotic resistance profile of E.coli strains isolated from clinical specimens and food samples in Egypt. Intl J Microbiol Res.2012;3(3):176-82.
Wayne PA. Clinical and laboratory standard institute 2006. Performance standards for antimicrobial disc tests. Approved Standards, 9th ed.; sixteenth informational supplement M2-M9. 2006;26.
Donskey CJ. Antibiotic regimen and intestinal colonization with antibiotic resistant gram negative bacilli. Antibiotics and gram negative bacilli.CID.2006Sep;43(S2):S64-9. DOI: https://doi.org/10.1086/504481.
Peña C, Pujol M, Ardanuy C, Ricart A, Pallares R, Liñares J, Ariza J, Gudiol F. Epidemiology and successful control of a large outbreak due to Klebsiella pneumoniae producing extended-spectrum beta-lactamases. Antimicrob Agents Chemother. 1998 Jan;42(1):53-8.
Olson B, Weinstein RA, Nathan C, Chamberlin W, Kabins SA. Epidemiology of endemic Pseudomonas aeruginosa: why infection control efforts have failed. J Infect Dis. 1984 Dec;150(6):808-16.
Lucet JC, Decré D, Fichelle A, Joly-Guillou ML, Pernet M, Deblangy C, Kosmann MJ, Régnier B. Control of a prolonged outbreak of extended-spectrum beta-lactamase-producing enterobacteriaceae in a university hospital. Clin Infect Dis. 1999 Dec;29(6):1411-8.
Wiener J, Quinn JP, Bradford PA, Goering RV, Nathan C, Bush K, Weinstein RA. Multiple antibiotic-resistant Klebsiella and Escherichia coli in nursing homes. JAMA. 1999 Feb 10;281(6):517-23.
Freter R, Brickner H, Fekete J, Vickerman MM, Carey KE. Survival and implantation of Escherichia coli in the intestinal tract. Infect Immun. 1983 Feb;39(2):686-703.
Shakya P, Barett P, Diwan V, Marothi Y, Shah H, Chhari N, et al. Antibiotic resistance among E coli isolates from stool samples of children aged 3 to 14 years from Ujjain, India. BMC Infectious diseases.2013Oct;13:477-83.DOI: https://doi.org/10.1186/1471-2334-13-477.
Cho SH, Lim Sl, Park SL, Kim SH, Kang YE. Prevalence of antibiotic resistance in Escherichia coli fecal isolates from healthy patients and patients with diarrhoea. Public health Res Prespect. 2011;2(1):41-5.Doi-https://doi.org/10.1016/j.phrp.2011.05.003.
Malakar M. Antimicrobial susceptibility pattern of Escherichia coli isolated from urine and stool samples of infected patients in Lakihmpur district of Assam, India. International Journal of Innovative Science, Engineering & technology.2014;1(2):184-9.
Rathaur VK, Pathania M,Jayara A,Yadav N. Clinical study of acute childhood diarrhea caused by bacterial Enteropathogens.J Clin Diag Res. 2014;8(5):PC)01-5.DOI: https://dx.doi.org/10.7860%2FJCDR%2F2014%2F6677.4319.
Hassani M. The Crisis of Resistant Gram Negative Bacterial Infection: Is there any Hope for ESKAPE?.Clin Res Infect Dis.2014;1(1):1005-9.
Hooper DC. Emerging mechanisms of fluoroquinolone resistance. Emerg Infect Dis. 2001 Mar-Apr;7(2):337-41.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


