Prevalence of invasive Trichosporonosis by Trichosporon asahii and other Trichosporon species and their antifungal susceptibility pattern in Chhattisgarh
Abstract
Introduction: Trichosporonosis is usually known to cause superficial mycoses, but now it is emerged as an opportunistic infectious disease. Trichosporon species is fairly uncommon fungus but can cause fatal mycosis in immunocompromised patients.
Objective: This study is an attempt to know prevalence of invasive trichosporonosis and its antifungal susceptibility.
Materials and Methods: All patients with a culture that was positive for Trichosporon species from February 2012 to February 2015 were included. Routine mycology works up done and suspected Trichosporon sp. were confirmed by automated miniAPI system. Antifungal susceptibility test was done for Fluconazole (F), Itraconazole(Itr), Voriconazole(V), Flucytosine(5Fc), AmphotericinB (AMB) done by minimum inhibitory concentration (MIC) method by ATB Fungus3 ( Biomerieux, France).
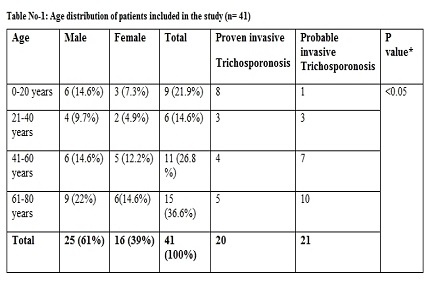
Result: 41 Trichosporon sp. was isolated from clinical specimen. Trichosporon asahii was the most common isolate (29 out of 41, 70.7%), followed by T. mucoides (5 of 41, 12.2%), T. inkin (2 of 41, 4.9%) and other Trichosporon sp. (5 out of 41,12.2%). Out of 41, 20 cases were proven to cause invasive trichosporonosis. Most invasive infections were associated with indwelling catheter (95%), associated bacterial infection(85%), ICU stay (85% each), prior antibiotic use (75%), cancer (65%), neutropenia, steroid use (55% each) and chemotherapy(50%). Amphotericin B was less susceptible against Trichosporon isolates whereas azole had good in vitro activity. Sensitivity of T.asahii towards Fluconazole, Itraconazole, Voriconazole, Amphotericin B and Flucytosine was 72.4%, 51.7%, 86.2%, 51.7% and 66.8% respectively.
Conclusion: T. asahii and other unusual Trichosporon sp.species also cause invasive trichosporonosis. For optimal therapy for trichosporonosis azoles can play a potential role.
Downloads
References
Chander J. Text book of Medical Mycology. 3rd Ed. Mehta publishers; 2009. Chapter 1, Introduction;p.2-18.
Pffaler M, Diekema D. Epidemiology of Invasive Candidiasis: A Persistent Public Health Problem. Clin Microbiol Rev. 2007; 20(1) :133-63.
Pradhan S, Singh S, Samal M.P., Murthy R, Pandey S. Characterization and Antifungal Susceptibility Pattern of Candida spp. Isolated from Clinical Specimens. J of Evolution of Med and Dent Sci. 2015; 4, Issue 40: 7004-7012.DOI: https://doi.org/10.14260/jemds/2015/1017.
Chowdhary A, Ahmad S, Khan Z U, Doval D C, Randhwa H S. Trichosporon asahii as an emerging etiologic agent of disseminated Trichosporonosis: A case report and an update. Ind J Med Microbiol,2004:22:16-22.
William G. Merz and Roderick J. Hay. Topley & Wilsons Microbiology and Microbial Infections : Medical Microbiology. 10th edition; Wiley Publication; 2005. Chapter 31, Serious Infections caused by uncommon yeasts : 624-635.
Middlehoven WJ. Identification of clinically relevant Trichosporon species. Mycoses.2003; 46:7-11.
Fisher F, Cook N. Fundamentals of Diagnostic Mycology, Saunders, 1998: 196-230.
Chander J. Text book of Medical Mycology, 3rd Ed. Mehta publishers; 2009. Chapter 26, Miscellaneous Oppotunistic Mycoses;p 387-398.
Chagas-Neto TC, Chaves GM, Colombo AL. Update on the genus Trichosporon. Mycopathologia. 2008 Sep;166(3):121-32. doi: https://doi.org/10.1007/s11046-008-9136-x. Epub 2008 Jun 21.
Ahmad S, AL – Mahmeed M, Khan ZU. Characterization of Trichosporon Species isolated from clinical specimens in Kuwait. J. Med Microbiol . 2005; 54: 639-46.
Pini G, Faggi E, Donato R, Fanci R. Isolation of Trichosporon in a hematology ward. Mycoses. 2005; 48:45-9.
Krcmery V Jr, Mateicka F, Kunova A et al,Haematogenous Trichosporonosis in cancer patient: Report of 12 cases including 5 during prophylaxis with Itraconazole. Support care cancer 1999; 7: 39-43.
De Pauw B, Walsh TJ, Donnelly JP, et al. Revised Definitions of Invasive Fungal Disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2008;46(12):1813-1821. doi: https://doi.org/10.1086/588660.
Rex JH, Pfaller MA, Walsh TJ, Chaturvedi V, Espinel-Ingroff A, Ghannoum MA, Gosey LL, Odds FC, Rinaldi MG, Sheehan DJ, Warnock DW. Antifungal susceptibility testing: practical aspects and current challenges. Clin Microbiol Rev. 2001 Oct;14(4):643-58, table of contents.
Pfaller MA, Diekema DJ, Rex JH, et al. Correlation of MIC with Outcome forCandida Species Tested against Voriconazole: Analysis and Proposal for Interpretive Breakpoints. Journal of Clinical Microbiology. 2006;44(3):819-826. doi: https://doi.org/10.1128/JCM.44.3.819-826.2006.
CLSI (2008a) Reference Method for Broth dilution Antifungal Susceptibility Testing of yeasts; approved standard –third edition; CLSI document M27-A3. Clinical and Laboratory Standards Institute, Wayne.
Sugita T, Nakajima M, Ikeda R, Matsushima T, Shinoda T. Sequence analysis of the ribosomal DNA intergenic spacer 1 regions of Trichosporon species. J Clin Microbiol. 2002 May;40(5):1826-30.
Kalkanci A., Sugita T, Arikan S, Yucesoy M, Ener B, Otag F, Kiraz N. et al. Molecular identification, genotyping, and drug susceptibility of the basidiomycetous yeast pathogen Trichosporon isolated from Turkish patients. Med Mycol. 2010 Feb; 48(1):141-6. doi: https://doi.org/10.3109/13693780902977984.
Sugita T, Nakajima M, Ikeda R, Matsushima T, Shinoda T. Sequence analysis of the ribosomal DNA intergenic spacer 1 regions of Trichosporon species. J Clin Microbiol. 2002 May;40(5):1826-30.
Chagas-Neto T.C., Chaves G.M., Melo A.S., Colombo A.L. Bloodstream infections due to Trichosporon spp.: species distribution, Trichosporon asahii genotypes determined on the basis of ribosomal DNA intergenic spacer 1 sequencing, and antifungal susceptibility testing. J ClinMicrobiol. 2009 Apr; 47(4): 1074–1081.
Girmenia, C., L. Pagano, B. Martino, D. D’Antonio, R. Fanci, G. Specchia, L. Melillo, M. Buelli, G. Pizzarelli, M. Venditti, and P. Martino. Invasive infections caused by Trichosporon species and Geotrichum capitatum in patients with hematological malignancies: a retrospective multicenter study from Italy and review of the literature. J. Clin. Microbiol. . 2005 Apr; 43(4): 1818–1828.doi: https://doi.org/10.1128/JCM.43.4.1818-1828.2005.
Vashishtha VM, Mittal A, Garg A. A fatal outbreak of Trichosporon asahii sepsis in a neonatal intensive care Unit. Indian Pediatr. 2012 Sep;49(9):745-7.
Khan ID, Sahni AK, Basu A, Haleem S. Trichosporon asahii urinary tract infection in immunocompetent patients. Med J Armed Forces India. 2015 Oct;71(4):373-6. doi: https://doi.org/10.1016/j.mjafi.2014.08.013. Epub 2014 Nov 6.
Sood S, Pathak D, Sharma R, Rishi S. Urinary tract infection by Trichosporon asahii. Indian J Med Microbiol. 2006 Oct;24(4):294-6.
Wolf DG, Falk R, Hacham M, Theelen B, Boekhout T, Scorzetti G, Shapiro M, Block C, Salkin IF, Polacheck I. Multidrug-resistant Trichosporon asahii infection of nongranulocytopenic patients in three intensive care units. J Clin Microbiol. 2001 Dec;39(12):4420-5.
Saad J. Taj-Aldeen, Naseer Al-Ansari, Sittana El Shafei, Jacques F. Meis, Ilse Curfs-Breuker et al. Molecular Identification and Susceptibility of Trichosporon Species Isolated from Clinical Specimens in Qatar: Isolation of Trichosporon dohaense Taj-Aldeen, Meis & Boekhout ap.nov J Clin. Microbiol. 2009 ;47(6):1761-1799.
Walsh TJ, Melcher GP, Lee JW, Pizzo PA. Infections due to Trichosporon species: new concepts in mycology, pathogenesis, diagnosis and treatment. Curr Top Med Mycol 1993; 5:79–113.
Colombo AL, Padovan AC, Chaves GM. Current knowledge of Trichosporon spp. and Trichosporonosis. Clin Microbiol Rev. 2011 Oct;24(4):682-700. doi: https://doi.org/10.1128/CMR.00003-11.
Rodriguez-Tudela JL, Diaz-Guerra TM, Mellado E, Cano V, Tapia C, Perkins A, Gomez-Lopez A, Rodero L, Cuenca-Estrella M. Susceptibility patterns and molecular identification of Trichosporon species. Antimicrob Agents Chemother. 2005 Oct;49(10):4026-34.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


