Comparison of local anaesthesia versus spinal anaesthesia for peri anal disorders
Abstract
Background: Peri anal disorders are associated with high morbidity and can be managed surgically both under spinal as well as local anaesthesia.
Objectives: The study evaluates the results of anal surgery when performed under local anaesthesia as compared to spinal anaesthesia with respect to parameters like post operative pain, nausea, vomiting, analgesia requirement, voiding problem and bleeding.
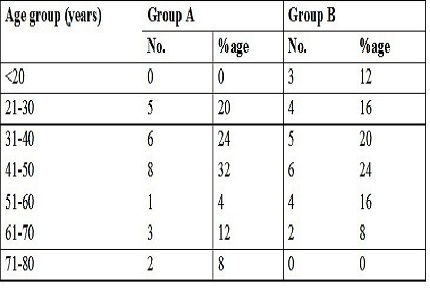
Material and Methods: The study included 50 patients divided in two groups (A and B) of 25 each. The patients of group A and group B were operated under local and spinal anaesthesia respectively. The patients were assessed postoperatively at 6 hrs, 8 hrs and 12 hrs on day one and then on subsequent days for different parameters like post operative pain, need and duration of analgesia required, bleeding, voiding problems and associated nausea.
Result: The results of two groups were then compared and analysed. In group A 56% of patients required analgesia 8 hourly as compared to 40% in group B. No analgesics were required 3 days after the surgery in both the groups. Difficulty in voiding was seen in 12% of patients in group A as compared to 28% in group B. There was no post operative bleeding except for 4 patients in group A. Most of the patients of group A had hospital stay of 2.3±0.46 days postoperatively while those in group B stayed for 3.4±0.53 days.
Conclusion: The study reveals favoured local anaesthesia over spinal anaesthesia for peri anal surgeries because of simplicity in administration of anaesthetic agent, less need of analgesia, lesser hospital stay, lesser incidence of nausea and vomiting and no need for catheterisation.
Downloads
References
Schneider HC. Hyaluronidase with local anesthesia in anorectal surgery. Am J Surg. 1954 Nov;88(5):703-6.
Sheikh P. Day care surgery-revised. Anorectal Surgery- Day Care is the New Mantra. Bombay Hospital Journal 2003;327:1324.
Dripps RD, Eckenhoff JE, Vandam LD. Introduction to anesthesia. The principles of safe practice. 6th Ed. Philadelphia: W.B Saunders Company 1982; 225.
Gopal DV. Diseases of the rectum and anus: a clinical approach to common disorders. Clin Cornerstone. 2002;4(4):34-48.
Haefeli M, Elfering A. Pain assessment. Eur Spine J. 2006 Jan;15 Suppl 1:S17-24. Epub 2005 Dec 1.
Surgery for colorectal cancer. American Cancer Society. Available from https://www.cancer.org/cancer/colon-rectal-cancer/treating/colon-surgery.html. Downloaded date 06-03-2017.
Gupta PJ. A review of proctological disorders. Eur Rev Med Pharmacol Sci. 2006 Nov-Dec;10(6):327-35.
Qureshi S, Aziz T, Afzal A, Maher M. Rubber band ligation of symptomatic Internal haemorrhoids; result of 450 Cases. Journal of Surgery Pakistan (International). 2009 Jan;14 (1); 19-22.
Lorenzo-Rivero S. Hemorrhoids: diagnosis and current management. Am Surg. 2009 Aug;75(8):635-42.
Hemorrhoids. America Society of Colon and Rectal Surgeons. Available from https://www.fascrs.org/publication/management-hemorrhoids. Downloaded date 06-03-2017.
Kaidar-Person O, Person B, Wexner SD. Hemorrhoidal disease: A comprehensive review. J Am Coll Surg. 2007 Jan;204(1):102-17. Epub 2006 Oct 25.
Hussain JN. Hemorrhoids. Prim Care 1999;26:25-51.
Mohsen S, Kashani T, Lak M, Mohebi HA and Panahe F. Lateral internal sphincterotomy under local anaesthesia: a randomized clinical trial. MJIR 2006;20(1):37-40.
Park SJ, Choi SI, Lee SH, Lee KY. Local perianal block in anal surgery. The disadvantage of pain during injfection despite high patient satisfaction. J Korena Surg Soc 2010;78(2):108.
Alatise OI, Agbakwurul AE, Takure AO, Adisa AO, Akinkuolie AA. Open hemorrhoidectomy under local anesthesia for symptomatic hemorrhoids; our experience in Ile–Ife, Nigeria. African Journal of Health Sciences. 2010 Jul;17(3&4):42-6.
Myles PS, Williams DL, Hendrata M, Anderson H, Weeks AM. Patient satisfaction after anaesthesia and surgery: results of a prospective survey of 10,811 patients. Br J Anaesth 2000 Jan 1;84(1):6-10.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


