Epidemiological profile of poisoning patients in the emergency department of a tertiary care teaching hospital in South India
Abstract
Background: Poisoning is a global public health issue and one of the common causes for visiting an emergency department (ED). A high index of suspicion based on etiology and clinical features is required to diagnose different types of poisons and their compounds.
Aims: To define the epidemiological profile of patients registered in the ED with complaints of ingestion of poison, and to identify different types of poisons consumed, the duration of hospital stay and mortality due to these poisons.
Methods: A retrospective analysis of patients presenting to the ED with complaints of poisoning. All patients registered in the ED with complaints of consumption of poison were included in the investigation. Patient charts with snake bites or scorpion stings were excluded. The medical charts with a discharge diagnosis of Poisoning during the study period were identified using the ICD-10-CM diagnosis codes categories T36-T65. Data was collected in a preformatted questionnaire.
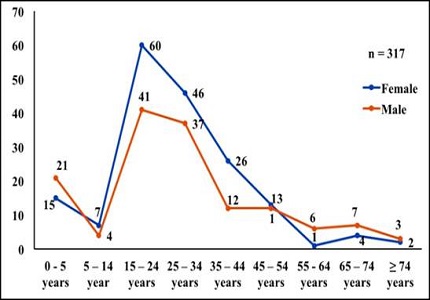
Results: In this study, 317 patients were enrolled, with a female predominance of 54.8%. Thirty-one percent of the patients are 15 to 24 years old, and 11.35% are below five years. Thirty percent were students, 18.3% housewives and 6.62% were farmers, with 59.3% having access to poisons at their homes, 19.87% from the pharmacy and 14.9% from a neighborhood store. The intent of poisoning in 85.8% of the patients was suicidal. 34.7% patients ingested pesticides, 30.28% patients, presented with tablet overdose, 14.82% patients consumed rodenticides and insecticides, and 3.47% patients presented with oleander seed poisoning. About 32.17% of the patients were admitted to ICU. Nearly 53.94% patients were discharged within three days of hospitalization. The mortality rate due to poisoning was 4.1%.
Conclusion: This research article defines the epidemiological profile of poisoning patients registered in the emergency department, along with the common poisons used, duration of hospital stay and mortality due to poisoning.
Downloads
References
Watson WA, Litovitz TL, Klein-Schwartz W, Rodgers GC Jr, Youniss J, Reid N, Rouse WG, Rembert RS, Borys D. 2003 Annual report of the American Association of Poison Control Centers Toxic Exposure Surveillance System. Am J Emerg Med. 2004 Sep;22(5):335-404.
Akkose S, Fedakar R, Bulut M, Armagan E, Cebicci H. Acute poisoning in adults in the years 1996–2001 treated in the Uludag University Hospital, Marmara Region, Turkey. Clin Toxicol 2005 Jan 1;43(2):105-109. DOI: https://doi.org/10.1081/CLT-50429.
Hanssens Y, Deleu D, Taqi A. Etiologic and demographic characteristics of poisoning: a prospective hospital-based study in Oman. J Toxicol Clin Toxicol. 2001;39(4):371-80.
Bruyndonckx RB, Meulemans AI, Sabbe MB, Kumar AA, Delooz HH. Fatal intentional poisoning cases admitted to the University Hospitals of Leuven, Belgium from 1993 to 1996. European Journal of Emergency Medicine 2002 Sep 1;9(3):238-243. PMID: 12394620.
Hatzitolios AI, Sion ML, Eleftheriadis NP, Toulis E, Efstratiadis G, Vartzopoulos D, et al. Parasuicidal poisoning treated in a Greek medical ward: epidemiology and clinical experience. Hum Exp Toxicol 2001 Dec;20(12):611-617. DOI: https://doi.org/10.1191%2F096032701718890595.
Burillo-Putze G, Munne P, Dueñas A, Pinillos MA, Naveiro JM, Cobo J, Alonso J; Clinical Toxicology Working Group, Spanish Society of Emergency Medicine (SEMESTOX). National multicentre study of acute intoxication in emergency departments of Spain. Eur J Emerg Med. 2003 Jun;10(2):101-4.
Goksu S, Yildirim C, Kocoglu H, Tutak A, Oner U. Characteristics of acute adult poisoning in Gaziantep, Turkey. J Toxicol Clin Toxicol. 2002;40(7):833-7.
Lamireau T, Llanas B, Kennedy A, Fayon M, Penouil F, Favarell-Garrigues JC, Demarquez JL. Epidemiology of poisoning in children: a 7-year survey in a paediatric emergency care unit. Eur J Emerg Med. 2002 Mar;9(1):9-14.
Tüfekçi IB, Curgunlu A, Sirin F. Characteristics of acute adult poisoning cases admitted to a university hospital in Istanbul. Hum Exp Toxicol. 2004 Jul;23(7):347-51.
Fernando R. The National Poisons Information Centre in Sri Lanka: the first ten years. J Toxicol Clin Toxicol. 2002;40(5):551-5.
Oxford English Dictionary. [Internet]. 2015. "poison, n.". Available at: http://www.oed.com/viewdictionaryentry/Entry/146669. Accessed February 19th, 2017.
Lau FL. Emergency management of poisoning in Hong Kong. Hong Kong Med J. 2000 Sep;6(3):288-92.
Staikowsky F, Theil F, Mercadier P, Candella S, Benais JP. Change in profile of acute self drug-poisonings over a 10-year period. Hum Exp Toxicol. 2004 Nov;23(11):507-11.
Singh D, Jit I, Tyagi S. Changing trends in acute poisoning in Chandigarh zone: a 25-year autopsy experience from a tertiary care hospital in Northern India. The American Journal of Forensic Medicine and Pathology 1999 Jun 1;20(2):203-210. PMID: 10414665.
Sharma BR, Harish D, Sharma V, Vij K. Poisoning in Northern India: changing trends, causes and prevention thereof. Medicine, science and the law 2002 Jul 1;42(3):251-257. PMID: 12201071.
Ab Rahman AF. Drug and chemical poisoning admissions at a teaching hospital in Malaysia. Hum Exp Toxicol 2002 July 1;21(7):377-381. PMID: 12269700.
Van Der Hoek W, Konradsen F. Risk factors for acute pesticide poisoning in Sri Lanka. Tropical Medicine & International Health 2005 Jun 1;10(6):589-596. DOI: https://doi.org/10.1111/j.1365-3156.2005.01416.x
Hwang K, Lee E, Hong S. Paraquat intoxication in Korea. Archives of Environmental Health: An International Journal 2002 Mar 1;57(2):162-166. DOI: https://doi.org/10.1080/00039890209602931.
Dong X, Simon MA. The epidemiology of organophosphate poisoning in urban Zimbabwe from 1995 to 2000. International journal of occupational and environmental health 2001 Oct 1;7(4):333-338. DOI: https://doi.org/10.1179/107735201800339191.
Kondle Raghu PS, Kumar SS, Gopal S, Shaik MV, Ahammed B. Incidence and Outcome of Poisoning Patients in a Tertiary Care Teaching Hospital. Asian Journal of Pharmacology and Toxicology 2015 Feb 25;3(7):23.
National Crime Records Bureau. Accidental death and suicides in India 2015. National Crime Records Bureau 2016 August 1:192-206.
Zine KU, Mohanty AC. Pattern of acute poisoning at Indira Gandhi Medical College and Hospital, Nagpur. J Ind Aca For Med 1998 Apr;20(2):37-39.
World Health Organization. Guidelines for poison control. 1st ed. Geneva: World Health Organization (WHO); 1997. ISBN: 9241544872.
Litovitz TL, Klein-Schwartz W, Caravati EM, Youniss J, Crouch B, Lee S. 1998 Annual report of the American Association of Poison Control Centers toxic exposure surveillance system. Am J Emerg Med 1999 Sep 1;17(5):435-487. PMID: 10496515.
Fingerhut LA, Cox CS. Poisoning mortality, 1985-1995. Public Health Rep. 1998 May-Jun;113(3):218-33.
Unnikrishnan B, Singh B, Rajeev A. Trends of acute poisoning in South Karnataka. Kathmandu Univ Med J (KUMJ). 2005 Apr-Jun;3(2):149-54.
Narayana Reddy KS. Toxicology, General consideration. 29th ed. New Delhi: Jaypee Brothers Medical Publishers; 2010.
Miller TR, Finkelstein AE, Zaloshnja E, Hendrie D. The cost of child and adolescent injuries and the savings from prevention. In: Karen DeSafey Liller, editor. Injury prevention for children and adolescents: research, practice, and advocacy. 1st ed. Washington DC: American Public Health Association; 2006. p. 15-64. ISBN: 978-0-87553-005-5.
Stevens JA, Corso PS, Finkelstein EA, Miller TR. The costs of fatal and non-fatal falls among older adults. Inj Prev. 2006 Oct;12(5):290-5.
Thomas SH, Bevan L, Bhattacharyya S, Bramble MG, Chew K, Connolly J, Dorani B, Han KH, Horner JE, Rodgers A, Sen B, Tesfayohannes B, Wynne H, Bateman DN. Presentation of poisoned patients to accident and emergency departments in the North of England. Hum Exp Toxicol. 1996 Jun;15(6):466-70.
McCaig LF, Burt CW. Poisoning-related visits to emergency departments in the United States, 1993-1996. J Toxicol Clin Toxicol. 1999;37(7):817-26.
Bajracharya MR, Deo KMK, Pahari SK. Age and gender distribution in deliberate self-poisoning cases. Post-Graduate Medical Journal of NAMS 2008 Jun 1;8(01).
Paudyal BP. Poisoning : Pattern and profile of admitted cases in a hospital in Central Nepal. JNMA J Nepal Med Assoc. 2005 Jul-Sep;44(159):92-6.
Gloglu C, Kara IH. Acute poisoning cases admitted to a university hospital emergency department in Diyarbakir, Turkey. Hum Exp Toxicol 2005 Feb;24(2):49-54. DOI: https://doi.org/10.1191%2F0960327105ht499oa.
Ozköse Z, Ayoglu F. Etiological and demographical characteristics of acute adult poisoning in Ankara, Turkey. Hum Exp Toxicol. 1999 Oct;18(10):614-8.
Xiang Y, Zhao W, Xiang H, Smith GA. ED visits for drug-related poisoning in the United States, 2007. Am J Emerg Med. 2012 Feb;30(2):293-301. doi: https://doi.org/10.1016/j.ajem.2010.11.031. Epub 2011 Mar 2.
Kanchan T, Menezes RG. Mortalities among children and adolescents in Manipal, Southern India. J Trauma. 2008 Jun;64(6):1600-7. doi: https://doi.org/10.1097/TA.0b013e3180a032a1.
Kanchan T, Menezes RG, Kumar TM, Bakkannavar SM, Bukelo MJ, Sharma PS, et al. Toxicoepidemiology of fatal poisonings in Southern India. Journal of forensic and legal medicine 2010 Aug;17(6):344-347. PMID:20650426.
Sinha US, Kapoor AK, Agnihotri AK, Srivastava PC. A profile of poisoning cases admitted in SRN Hospital, Allahabad with special reference to aluminium phosphide poisoning. Journal of Forensic Medicine & Toxicology 1999 Jun 1;16(1):43-42. ISSN: 0972-0448.
Senanayake N, Peiris H. Mortality due to poisoning in a developing agricultural country: trends over 20 years. Hum Exp Toxicol. 1995 Oct;14(10):808-11.
Dhattarwal SK, Dalal SS. Profile of deaths due to poisoning in Rohtak, Haryana in the year 1995. Journ Forensic Med Toxicol 1997;14:51.
Sheikh MI, Agarwal SS, Kumar L, Jhaveri S. Changing trends of poisoning in Surat. International Journal of Medical Toxicology & Legal Medicine 2004 Jun;6(2):17-21. ISSN:0972-0448.
Banerjee I, Tripathi SK, Roy AS. Clinico-epidemiological characteristics of patients presenting with organophosphorus poisoning. North American journal of medical sciences 2012 Mar 1;4(3):147. PMID: 22454830.
Ramesha KN, Rao KB, Kumar GS. Pattern and outcome of acute poisoning cases in a tertiary care hospital in Karnataka, India. Indian J Crit Care Med. 2009 Jul-Sep;13(3):152-5. doi: https://dx.doi.org/10.4103%2F0972-5229.58541.
Abdollahi M, Jalali N, Sabzevari O, Hoseini R, Ghanea T. A retrospective study of poisoning in Tehran. J Toxicol Clin Toxicol. 1997;35(4):387-93.
Zaheer MS, Aslam M, Gupta V, Sharma V, Khan SA. Profile of poisoning cases at a North Indian tertiary care hospital. Health Popul Perspect Issues 2009;32:176-183.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


