Characteristics of multi drug resistant tuberculosis cases at a selected tertiary level hospital
Abstract
Background: This study was carried out to determine the characteristics of MDR-TB cases under treatment at National Institute of Diseases of the Chest and Hospital (NIDCH), Mohakhali, Dhaka.
Methods: This was a descriptive cross sectional study among 442 diagnosed MDR-TB patients admitted in NIDCH of which 303 MDR-TB patients were included as respondents. The respondents were selected purposively and they were interviewed with duly pre-tested research instruments.
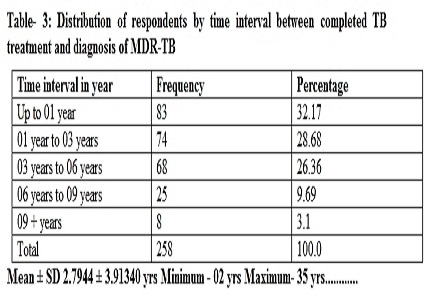
Results: Among the study populations (303), all were resistant to H & R and 149 (57.7%) consumed standard drugs regimen contained H, R, E & S. In addition the factors related to develop MDR-TB mostly as non-compliance, overcrowding and exposure to MDR-TB were 190 (73.7%), 261 (86.1%) and 81 (26,7%) respectively. In this study, time interval between completed anti-TB treatment and diagnosis of MDR-TB found 01 to 06 years among 55.4% respondents. Moreover tools used for diagnosis of MDR-TB were found in 258 (85.1%) as smear for AFB, Gene expert tests and Culture. Age group 16 to 30 yrs 184 (60.7%), income group 10001 to 20000 taka per month 143 (47.2%), educational qualification class VI-X 72 (23.8%) and urban population 180 (59.4%) were affected more. The association between type of house, crowding status and occurrence of MDR-TB were found statistically significant (p<0.05) but source of drugs, compliance of treatment, availability of drugs and occurrence of MDR-TB shown statistically highly significant, (p<.001). Correlation with age, family income and time gap of diagnosis MDR-TB was statistically significant (p<0.05). Principal.
Conclusion: Study findings demands establishment of standard diagnostics procedures/laboratories at all secondary and tertiary care hospitals and TB clinics in the country in support of uniformity of intervention therapy.
Downloads
References
Park, k, (2011). Park,s Textbook of Preventive and Social Medicine; “Epidemiology of Communicable Diseases, Tuberculosis”, 21st edition, India, Banarsidas Bhanot publisher,2011, p-159, 162.
Zignol M, Dara M, Dean AS, Falzon D et al. Drug-resistant tuberculosis in the WHO European Region: An analysis of surveillance data. Drug Resist Update Rev Comment Antimicrob Anticancer Chemother. 2013; 16(6):108-15.
Menon Sarala, Dharmshale Sujata, Chande Chhaya. Drug resistance profiles of Mycobacterium tuberculosis isolates to first line anti-tubercular drugs: A five years study (2005-2009). J Health Popul Nutr. Feb 2010; 28(1): 7–13. v
Gandhi NR, Andrews JR, Brust JC, Montreuil R, Weissman D, Heo M, Moll AP, Friedland GH, Shah NS. Risk factors for mortality among MDR- and XDR-TB patients in a high HIV prevalence setting. Int J Tuberc Lung Dis. 2012 Jan;16(1):90-7. doi: https://doi.org/10.5588/ijtld.11.0153.
Zarir F Udwadia, Gautam Moharil. Multidrug-resistant-tuberculosis treatment in the Indian private sector: Results from a tertiary referral private hospital in Mumbai. Web Publication, Department of Pulmonology, Hinduja Hospital and Research Center, Mumbai, Maharashtra, India, Volume:31, Issue:4, Page:336-341.
Gupta A, Nagaraja MR, Kumari P, Singh G, Raman R, Singh SK, Anupurb S. Association of MDR-TB isolates with clinical characteristics of patients from Northern region of India. Indian J Med Microbiol. 2014 Jul-Sep;32(3):270-6. doi: http://www.ijmm.org/text.asp?2014/32/3/270/136561.
Uzoewulu NG1, , Ibeh IN , Lawson L, Goyal M, et al. Mycobacterium tuberculosis in Tertiary Hospital South East, Nigeria. Journal of Medical Microbiology & Diagnosis, 3:141. doi: https://doi.org/10.4172/2161-0703.1000141, June 29, 2014.
Leung EC, Yew WW, Leung CC, Leung WM, et al. Shorter treatment duration for selected patients with multidrug-resistant tuberculosis. Eur Respir J. 2011;38(1):227–30.
Zaman K, Rahim Z, Yunus M, Arifeen S, Baqui A, Sack D, Hossain S, Banu S, Islam MA, Ahmed J, Breiman R, Black R. Drug resistance of Mycobacterium tuberculosis in selected urban and rural areas in Bangladesh. Scand J Infect Dis. 2005;37(1):21-6.
R Israt. A Study on Hematological Indices of Tuberculosis Patients Attending in a Tertiary Care Hospital in Dhaka City. Department of Pharmacy, East West University June, 2012.
Maurya AK, Singh AK, Kumar M, Umrao J, Kant S, Nag VL, Kushwaha RA, Dhole TN. Changing patterns and trends of multidrug-resistant tuberculosis at referral centre in Northern India: a 4-year experience. Indian J Med Microbiol. 2013 Jan-Mar;31(1):40-6. doi: http://www.ijmm.org/text.asp?2013/31/1/40/108720.
Flora MS, Amin MN, Karim MR, Afroz S, Islam S, Alam A, Hossain M. Risk factors of multi-drug-resistant tuberculosis in Bangladeshi population: a case control study. Bangladesh Med Res Counc Bull. 2013 Apr;39(1):34-41.
Dr Nirmalya Manna, Kajaree Giri, Dr Malay Mundle et al. Drug resistance pattern, related socio- demographic factors and preventive practices among MDR-TB patients: An experience from a tertiary care setting. IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) Volume 13, Issue 9, Ver. VI (Sep. 2014), PP 16-21.
Sethi Sunil, Mewara Abhishek, Kumar Dhatwalia Sunil, et al. Prevalence of multidrug resistance in Mycobacterium tuberculosis isolates from HIV seropositive and seronegative patients with pulmonary tuberculosis in north India. BMC Infectious Diseases 2013, 13:137 doi: https://doi.org/10.1186/1471-2334-13-137, 15 March 2013.
Kurniawati Fivy, azhar syed, sulaiman syed, gillani syed wasif et al. Study on drug-resistant tuberculosis and tuberculosis treatment on Patients with drug resistant tuberculosis in chest clinic outpatient Department”, International journal of pharmacy and pharmaceutical sciences, vol 4, issue 2, 2012, Issn- 0975-1491.
Jit Bahadur Darnal, Swaddiwudhipong W et al. Multidrug-resistant Tuberculosis Patients in Bhutan”, Department of Community and Social Medicine, Mae Sot General Hospital, Tak Province, Thailand August 2011 to July 2012 , OSIR, September 2013, Volume 6, Issue 3, p. 6-10 6.
Goswami Avranil, Chakraborty Urmita, Mahapatra Tanmay, et al. Correlates of Treatment Outcomes and Drug Resistance among Pulmonary Tuberculosis Patients Attending Tertiary Care Hospitals of Kolkata, India. PLoS ONE 9(10): e109563. doi: https://dx.doi.org/10.1371%2Fjournal.pone.0109563. October 7, 2014.
Helbling Peter, Altpeter Ekkehardt, Egger Jean-Marie et al. Treatment outcomes of multidrug-resistant tuberculosis in Switzerland. Swiss Med Wkly. 2014;144:w14053, 4 December 2014.
Banu Sayera, Mujtaba Mahmud Asif, Rahman Toufiq, et . Multidrug-Resistant Tuberculosis in Admitted Patients at a Tertiary Referral Hospital of Bangladesh. PLoS ONE 7(7): e40545. doi: https://doi.org/10.1371/journal.pone.0040545.
Lukoye Deus, Ssengooba Willy, Musisi Kenneth et al. Variation and risk factors of drug resistant tuberculosis in sub-Saharan Africa: a systematic review and meta-analysis”. BMC Public Health 2015, 15:291 doi: https://doi.org/10.1186/s12889-015-1614-8.
Khurram M, Khaar HT, Fahim M. Multidrug-resistant tuberculosis in Rawalpindi, Pakistan. J Infect Dev Ctries. 2012 Jan 12;6(1):29-32.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


