Polysomnographic Spectrum in Obstructive Sleep Apnoea
Abstract
Introduction: Obstructive sleep apnea (OSA) is a common sleep disordered breathing which is often undiagnosed, unrecognized and under treated represents a major public health problem. It is diagnosed by using overnight Polysomnography. The aim of the study was to analyse the Polysomnographic spectrum in Obstructive sleep apnea.
Methods: The study was prospective and observational type which included all patients diagnosed with OSA by overnight polysomnography (AHI≥5 events per hour) who had visited department of pulmonary medicine from September 2015 to August 2016. Their polysomnographic data with relevant clinical data were collected and analysed.
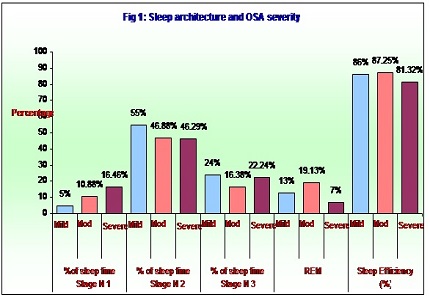
Results: The mean age of the study group was 49.74 ± 11.59. Our study showed males (41/50 82%) were predominant with male to female ratio of 4:1. Among 50 patients 41(82%) had severe OSA, 8 (16%) moderate and 1 (2%) with mild OSA. The architecture of sleep in OSA was disturbed; the amount of sleep spent in stage N1 had increased to 15.34±9.18, stage N2 and N3 varied and the amount of sleep spent in REM was decreased (9.06 ± 7.93) with varied sleep efficiency. Respiratory events were more in N3 and REM sleep. With CPAP there was definite increase in the stage N3 (P=0.010) and REM sleep (P=0.0000). There was reduction in RDI (P=0.0000).
Conclusion: Overnight polysomnography is the standard test recommended for diagnosis of OSA. OSA significantly affected the sleep architecture, sleep efficiency. Early diagnosis by regular sleep evaluation in routine clinical practice would result in better treatment outcome.
Downloads
References
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. New Engl J Med. 1993;328(17):1230–5.doi: https://doi.org/10.1056/nejm199304293281704.
Young T, Peppard P, Gottlieb D. Epidemiology of obstructive sleep apnea. Am J Respir Crit Care Med. 2002;165(9):1217-39.doi: https://doi.org/10.1164/rccm.2109080.
Gibson GJ. Obstructive sleep apnoea syndrome: underestimated and undertreated. Br Med Bull. 2005 Mar 29;72:49-65. Print 2004. doi: https://doi.org/10.1093/bmb/ldh044.
Duran J, Esnaola S, Rubio R, Iztueta A. Obstructive sleep apnea-hypopnea and related clinical features in a population-based sample of subjects aged 30 to 70 year. Am J Respir Crit Care Med. 2001;163:685-9.doi: https://doi.org/10.1164/ajrccm.163.3.2005065.
Schlosshan D, Elliott MW. Sleep . 3: Clinical presentation and diagnosis of the obstructive sleep apnoea hypopnoea syndrome. Thorax. 2004 Apr;59(4):347-52.doi: https://doi.org/10.1136/thx.2003.007179.
He J, Kryger MH, Zorick FJ, Conway W, Roth T. Mortality and apnea index in obstructive sleep apnea. Experience in 385 male patients. Chest. 1988 Jul;94(1):9-14.
Engleman HM, Douglas NJ. Sleep. 4: Sleepiness, cognitive function, and quality of life in obstructive sleep apnoea/hypopnoea syndrome. Thorax. 2004 Jul;59(7):618-22.doi: https://dx.doi.org/10.1136%2Fthx.2003.015867.
George C. Sleep {middle dot} 5: Driving and automobile crashes in patients with obstructive sleep apnoea/hypopnoea syndrome. Thorax. 2004;59(9):804-7.doi: http://dx.doi.org/10.1136/thx.2003.007187.
Sleep apnoea as an independent risk factor for cardiovascular disease: current evidence, basic mechanisms and research priorities. W.T. McNicholas, M.R. Bonsignore and the management committee of EU cost action B26. Eur Respir J. 2007;29:156-78.doi: https://doi.org/10.1183/09031936.00027406.
Carmal A. [Internet]. Emedicine.com. 2007 [cited 10 October 2016]. Available from: http://carmalapolysomnography:overviewandclinicalapplication.e-medicine.com2007.
SK S. Policy document consensus & evidence-based INOSA guidelines 2014 (First Edition). Journal of Clinical and Scientific Research.2015;:70-91.
American Academy of Sleep Medicine. International classification of sleep disorders. diagnostic and coding manual. Westchester, Illinois; AASM: 2005.
Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep. 1999 Aug 1;22(5):667-89.
Ryan CM, Bradley TD. Pathogenesis of obstructive sleep apnea. J Appl Physiol (1985). 2005 Dec;99(6):2440-50. doi: https://doi.org/10.1152/japplphysiol.00772.2005.
Harris CD. Neurophysiology of sleep and wakefulness. Respir Care Clin N Am. 2005 Dec;11(4):567-86.doi: https://doi.org/10.1016/j.rcc.2005.08.001.
Rechtschaffen A, Kales A: A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. Washington, DC: US Government Printing Office, US Public Health Service; 1968.
Russo M. [Internet]. e-medicine.com 2005 [cited 10 October 2016]. Available from: http://russomsleepstagescoringemedicine.com 2005.
Udwadia ZF, Doshi AV, Lonkar SG, Singh CI. Prevalence of sleep-disordered breathing and sleep apnea in middle-aged urban Indian men. Am J Respir Crit Care Med. 2004 Jan 15;169(2):168-73. Epub 2003 Nov 6.doi: https://doi.org/10.1164/rccm.200302-265oc.
Sharma SK, Kumpawat S, Banga A, Goel A. Prevalence and risk factors of obstructive sleep apnea syndrome in a population of Delhi, India. Chest. 2006 Jul;130(1):149-56.doi: https://doi.org/10.1378/chest.130.1.149.
Chaouat A, Weitzenblum E, Krieger J, Ifoundza T, Oswald M, Kessler R. Association of chronic obstructive pulmonary disease and sleep apnea syndrome. Am J Respir Crit Care Med. 1995;151:82-86.doi: https://doi.org/10.1164/ajrccm.151.1.7812577.
Sreedharan SE, Agrawal P, Rajith RS, Nair S, Sarma SP, Radhakrishnan A. Clinical and polysomnographic predictors of severe obstructive sleep apnea in the south indian population. Ann Indian Acad Neurol. 2016;19:216-20.doi: http://www.annalsofian.org/text.asp?2016/19/2/216/173315.
Garg R, Singh A, Prasad R, Saheer S, Jabeed P, Verma R. A comparative study on the clinical and polysomnographic pattern of obstructive sleep apnea among obese and non-obese subjects. Ann Thorac Med. 2012;7(1):26-30.doi: https://doi.org/10.4103/1817-1737.91561.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


