Prescription auditing based on World Health Organization (WHO) prescribing indicators in a teaching hospital in North India
Abstract
Background: Prescription writing is an important means of therapeutic intervention by the doctor and reflects his approach towards safe prescribing. Complacency in prescribing results in errors which can even cause adverse effects. These errors can be detected through a prescription audit. We undertook this study to audit the out-patient department (OPD) prescriptions for completeness of prescription format, legibility and against the World Health Organization (WHO) prescribing indicators recommended to investigate rational use of drugs.
Methods: OPD prescriptions were photographed from the pharmacy of a teaching hospital over a period of three months and 1274 prescriptions were audited. Prescriptions were evaluated for completeness of prescription format while legibility was graded as grade 1, 2 and 3. Prescriptions were also analyzed on the five WHO prescribing indicators.
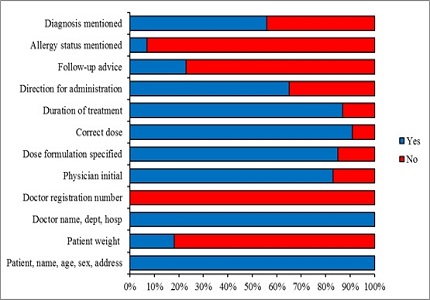
Results: An average of 4.02 ± 2.23 drugs were prescribed per prescription of which 39.01% were antibiotics. Though 79.2% drugs were prescribed from the Essential Drug List, none was prescribed by the generic name. Rate of injection use was 7.54% in our study. Registration number of the doctor was absent in 100% of the prescriptions. Errors such as omitting the mention of allergy status, follow-up advice and directions of use were common. Almost 8% prescriptions were illegible (grade3) and 66.8% were legible with difficulty (grade 2).
Conclusion: Majority of the prescriptions were incomplete and poly-pharmacy was evident in our study. Regular auditing and feedback is necessary for imbibing safe prescribing practices. Doctors need to be made aware about the errors and the recommended guidelines.
Downloads
References
Ross S, Bond C, Rothnie H, Thomas S, Macleod MJ. What is the scale of prescribing errors committed by junior doctors? A systematic review. Br J Clin Pharmacol. 2009 Jun;67(6):629-40. doi: https://doi.org/10.1111/j.1365-2125.2008.03330.x. Epub 2008 Oct 23.
Velo GP, Minuz P. Medication errors: prescribing faults and prescription errors. Br J Clin Pharmacol 2009;67(6):624-8. doi: https://doi.org/10.1111/j.1365-2125.2009.03425.x.
Reason J. Human error: models and management. BMJ 2000 Mar 18;320(7237):768-70.doi: https://doi.org/10.1136/bmj.320.7237.768.
Montesi G, Lechi A. Prevention of medication errors: detection and audit. Br J Clin Pharmacol 2009;67(6):651-655. doi: https://doi.org/10.1111/j.1365-2125.2009.03422.x.
National Institute for Clinical Excellence (NICE): Principles for Best Practice in Clinical Audit. Oxford: Radcliffe Publishing 2002.
World Health Organization:How to Investigate Drug Use in Health Facilities: Selected Drug Use Indicators - EDM Research Series. http://apps.who.int/medicinedocs/en/d/Js2289e/ (accessed 26 september 2016).
Shelat PR, Kumbar SK. Analysis of Out Door Patients Prescriptions According to World Health Organization (WHO) Prescribing Indicators Among Private Hospitals in Western India. J Clin Diagn Res 2015;9(3):FC01-4. doi: https://dx.doi.org/10.7860%2FJCDR%2F2015%2F12724.5632.
Abidi A, Gupta S, Kansal S. Prescription auditing and drug utilization pattern in a tertiary care teaching hospital of western UP. Int J Basic Clin Pharmacol. 2012; 1(3): 184-190. doi: https://doi.org/10.5455/2319-2003.ijbcp003812.
Seden K, Kirkham JJ, Kennedy T. Cross-sectional study of prescribing errors in patients admitted to nine hospitals across North West England. BMJ Open 2013;3:e002036. doi: http://dx.doi.org/10.1136/bmjopen-2012-002036.
Kiekkas P, Karga M, Lemonidou C, Aretha D, Karanikolas M. Medication errors in critically ill adults: A review of direct observation evidence. Am J Crit Care 2011;20(1):36-44. doi: https://doi.org/10.4037/ajcc2011331.
Model prescription format. http://www.delhimedicalcouncil.org/pdf/modalprescription.pdf (accessed 26 september 2016).
Albarrak AI, Al Rashidi EA, Fatani RK, Al Ageel SI, Mohammed R. Assessment of legibility and completeness of handwritten and electronic prescriptions. Saudi Pharm J. 2014 Dec;22(6):522-7. doi: https://doi.org/10.1016/j.jsps.2014.02.013. Epub 2014 Mar 13.
Potharaju HR, Kabra SG. Prescription audit of outpatient attendees of secondary level government hospitals in Maharashtra. Indian J of Pharmacol. 2011;43(2):150-6. doi: https://dx.doi.org/10.4103%2F0253-7613.77350.
Patil KR, Mali RS, Dhangar BK, Bafna PS, Gagarani MB, Bari SB. Assessment of Prescribing Trends and Quality of handwritten Prescriptions from Rural India.Journal of Pharma Scitech 2015;5(1):54-60. http://www.pharmascitech.in/admin/php/uploads/101_pdf.pdf
Kun Y, Jianwen C, Hua F, Huifen C, Yizhong Z. Analysis of factors affecting physician’s prescribing conduct. Chin J Hosp Admin 2002;18:92-4.
Hazra A, Tripathi SK, Alam MS. Prescribing and dispensing activities at the health facilities of a nongovernmental organization.Natl Med J India 2000 Jul-Aug;13:177-82.http://archive.nmji.in/archives/Volume-13/issue-4/original-articles-1.pdf.
El Mahalli AA. WHO/INRUD drug prescribing indicators at primary health care centres in Eastern province, Saudi Arabia. East Mediterr Health J Rev Santé Méditerranée Orient Al-Majallah Al-Ṣiḥḥīyah Li-Sharq Al-Mutawassiṭ 2012;18(11):1091–6.doi: https://doi.org/10.26719/2012.18.11.1091.
Agrawal A, Aronson JK, Britten N. Medication errors problems and recommendations from a consensus meeting. Br J Clin Pharmacol 2009 Jun;67(7):592-8. doi: https://doi.org/10.1111/j.1365-2125.2009.03414.x.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


