Safety and efficacy of percutaneous device closure of large post tricuspid shunts in pediatric patients with severe PAH at short term and midterm follow up
Abstract
Background: Transcatheter closure of large post-tricuspid shunts in patients with severe pulmonary arterial hypertension remains a challenging problem. Among this unique subset of patients there is an entire spectrum of severity of pulmonary vascular disease with variable pulmonary vascular resistance and reversibility especially in older children.
Aims: The current study was done to assess the safety and efficacy of percutaneous device closure of large post tricuspid shunts in pediatric patients with severe PAH at short and mid term follow up.
Methods: A total of 42 pediatric patients underwent transcatheter closure of large post tricuspid shunts with severe PAH. All subjects underwent clinical examination, electrocardiography, chest x-rays and echocardiography before discharge and at 1, 6 and 12 months after the procedure and yearly thereafter.
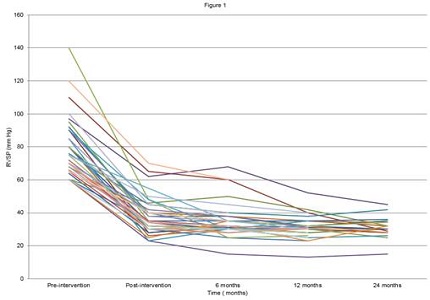
Results: Most of the patients (64 %) were having patent ductus arteriosus followed by ventricular septal defect in 8 patients (19.04%), aorto-pulmonary window in 5 patients (12%) and coronary cameral fistula in 2 patients (5%). Cardi-O-Fix VSD occluder was the most commonly used device (45%), Cardi-O-Fix PDA occluder (21%) and Amplatzer duct occluder in 17% patients. Pre-procedural pulmonary artery systolic pressure decreased significantly from mean 81.12 mmHg to mean 43.17 mmHg post procedure over a mean follow-up of 18.5 months. Only two major complications viz; severe aortic obstruction and symptomatic complete heart block were noticed in two children.
Conclusions: Our study showed that the transcatheter closure of large post tricuspid shunts in pediatric patients with severe PAH was safe, feasible and efficacious alternative to conventional surgery.
Downloads
References
Marelli AJ, Mackie AS, Ionescu-Ittu R, Rahme E, Pilote L. Congenital heart disease in the general population: changing prevalence and age distribution. Circulation. 2007;115:163-172.doi: https://doi.org/10.1161/circulationaha.106.627224.
Hoffman JI. Incidence of congenital heart disease: I. Postnatal incidence. Pediatr Cardiol. 1995 May-Jun;16(3):103-13.doi: https://doi.org/10.1007/bf00801907.
Adatia I, Kothari SS, Feinstein JA. Pulmonary hypertension associated with congenital heart disease: pulmonary vascular disease: the global perspective. Chest. 2010 Jun;137(6 Suppl):52S-61S. doi: https://doi.org/10.1378/chest.09-2861.
GROSS RE. Surgical closure of an aortic septal defect. Circulation. 1952 Jun;5(6):858-63.doi: https://doi.org/10.1161/01.cir.5.6.858.
SCOTT HW Jr, SABISTON DC Jr. Surgical treatment for congenital aorticopulmonary fistula; experimental and clinical aspects. J Thorac Surg. 1953 Jan;25(1):26-39.
COOLEY DA, MCNAMARA DG, LATSON JR. Aorticopulmonary septal defect: diagnosis and surgical treatment. Surgery. 1957 Jul;42(1):101-20; discussion, 120.
MORROW AG, GREENFIELD LJ, BRAUNWALD E. Congenital aortopulmonary septal defect. Clinical and hemodynamic findings, surgical technic, and results of operative correction. Circulation. 1962 Mar;25:463–476.doi: https://doi.org/10.1161/01.cir.25.3.463.
Johansson L, Michaelsson M, Westerholm CJ, Aberg T. Aortopulmonary window: a new operative approach. Ann Thorac Surg. 1978 Jun;25(6):564-7.doi: https://doi.org/10.1016/s0003-4975(10)63611-9.
Wright JS, Freeman R, Johnston JB. Aorto-pulmonary fenestration. A technique of surgical management. J Thorac Cardiovasc Surg. 1968 Feb;55(2):280-3.
Deverall PB, Lincoln JC, Aberdeen E, Bonham-Carter RE, Waterston DJ. Aortopulmonary window. J Thorac Cardiovasc Surg. 1969 Apr;57(4):479-86.
ELLIS FH Jr, KIRKLIN JW, CALLAHAN JA, WOOD EH. Patent ductus arteriosus with pulmonary hypertension; an analysis of cases treated surgically. J Thorac Surg. 1956 Mar;31(3):268-82; discussion, 282-5.
Shyamkrishnan KG, Singh M, Tharakan JM, Dal A. A ten-year post-surgical assessment of pulmonary hypertension in adults with patent ductus arteriosus. Indian Heart J. 1996 May-Jun;48(3):249-51.
Masura J, Walsh KP, Thanopoulous B, Chan C, Bass J, Goussous Y, Gavora P, Hijazi Z. Catheter closure of moderate-large sized patent ductus arteriosus using the new Amplatzer duct occluder: immediate and short-term results. J Am Coll Cardiol. 1998; 31:878-882.doi: https://doi.org/10.1016/s0735-1097(98)00013-8.
Fischer G, Stieh J, Uebing A, Grabitz R, Kramer HH. Transcatheter closure of persistent ductus arteriosus in infants using the Amplatzer duct occluder. Heart. 2001 Oct;86(4):444-7.doi: https://doi.org/10.1136/heart.86.4.444.
Thanapoulus BD, Tsaousis GS, Djukic M, Al Hakim F, Eleftherakis NG, Simeunovic SD. Transcatheter closure of high pulmonary pressure persistent ductus arteriosus with Amplatzer muscular ventricular septal defect occluder. Heart. 2002; 87:260-3.doi: https://dx.doi.org/10.1136%2Fheart.87.3.260.
Butera G, De Rosa G, Chessa M, Piazza L, Delogu A, Frigiola A, Carminati M. Transcatheter closure of persistent ductus arteriosus with the Amplatzer duct occluder in very young symptomatic children. Heart. 2004 Dec;90(12):1467-70.doi: https://doi.org/10.1136/hrt.2003.025122.
Roy A, Juneja R, Saxena A.Use of Amplatzer duct occluder to close severely hypertensive ducts: Utility of transient balloon occlusion. Indian Heart J. 2005; 57:332-6.
Sivakumar K, Francis E. Transcatheter closure of distal aortopulmonary window using Amplatzer device. Congenit Heart Dis. 2006 Nov;1(6):321-3. doi: https://doi.org/10.1111/j.1747-0803.2006.00055.x.
Wang JK, Wu MH, Hwang JJ, Chiang FT, Lin MT, Lue HC. Transcatheter closure of moderate to large patent ductus arteriosus with the Amplatzer duct occluder. Catheter Cardiovasc Interv. 2007 Mar 1;69(4):572-8.doi: https://doi.org/10.1002/ccd.20701.
Qiang J, Jing F, Yunqing M, Xisheng W, Jiangzhi C, Yifeng S. Transcatheter closure of adult patent ductus arteriosus with severe pulmonary hypertension. Hypertens Res. 2008; 31:1997–2002.https://www.nature.com/articles/hr2008252.pdf?origin=ppub.
Trehan V, Nigam A, Tyagi S. Percutaneous closure of non-restrictive aortopulmonary window in three infants. Catheter Cardiovasc Interv. 2008; 71:405-11.
Yang SW, Zhou YJ, Hu DY, Liu YY, Shi DM, Guo YH, Cheng WJ, Nie XM, Wang JL. Feasibility and safety of transcatheter intervention for complex patent ductus arteriosus. Angiology. 2010 May;61(4):372-6. doi: https://doi.org/10.1177%2F0003319709351874. Epub 2009 Nov 18.
Parra-Bravo R, Cruz-Ramírez A, Rebolledo-Pineda V, Robles-Cervantes J, Chávez-Fernández A, Beirana-Palencia L, Jiménez-Montufar L, Estrada-Loza Mde J, Estrada-Flores J, Báez-Zamudio N, Escobar-Ponce M. Transcatheter closure of patent ductus arteriosus using the amplatzer duct occluder in infants under 1 year of age. Rev Esp Cardiol. 2009 Aug;62(8):867-74.
Zabal C, García-Montes JA, Buendía-Hernández A, Calderón-Colmenero J, Patiño-Bahena E, Juanico-Enriquez A, Attie F. Percutaneous closure of hypertensive ductus arteriosus. Heart. 2010 Apr;96(8):625-9. doi: http://dx.doi.org/10.1136/hrt.2009.185025.
Castaldi B, Santoro G, Gaio G, Palladino MT, Iacono C, Russo MG. Transcatheter closure of symptomatic arterial duct in infants younger than 1 year old. Pediatr Cardiol. 2012 Dec;33(8):1397-401. doi: https://doi.org/10.1007/s00246-012-0356-y. Epub 2012 May 26.
Bhalgat PS, Pinto R, Dalvi BV. Transcatheter closure of large patent ductus arteriosus with severe pulmonary hypertension: short and intermediate term results. Ann Ped cardiol. 2012; 5:135–40.doi: http://www.annalspc.com/text.asp?2012/5/2/135/99614.
Garcia-Montes JA, Camacho-Castro A, Sandoval-Jones JP, Buendia-Hernandez A, Calderon-Colmenero J, Patino-Bahena E. Closure of large patent ductus arteriosus using the Amplatzer Septal Occluder. Cardiol Young. 2015; 25(3):491–5.doi: https://doi.org/10.1017/s1047951114000183.
Park YA, Kim NK, Park SJ, Yun BS, Choi JY, Sul JH. Clinical outcome of transcatheter closure of patent ductus arteriosus in small children weighing 10 kg or less. Korean J Pediatr. 2010; 53(12):1012-6.doi: https://doi.org/10.3345/kjp.2010.53.12.1012.
Galal MO, Amin M, Hussein A, Kouatli A, Al-Ata J, Jamjoom A. Left ventricular dysfunction after closure of large patent ductus arteriosus. Asian Cardiovasc Thorac Ann. 2005;13:24-9.doi: https://doi.org/10.1177/021849230501300106.
Eerola A, Jokinen E, Boldt T, Pihkala J. The influence of percutaneous closure of patent ductus arteriosus on left ventricular size and function: a prospective study using two- and three-dimensional echocardiography and measurements of serum natriuretic peptides. J Am Coll Cardiol. 2006 Mar 7;47(5):1060-6. Epub 2006 Feb 9.doi: https://doi.org/10.1016/j.jacc.2005.09.067.
Kim YH, Choi HJ, Cho Y, Lee SB, Hyun MC. Transient left ventricular dysfunction after percutaneous patent ductus arteriosus closure in children. Korean Circ J. 2008; 38:596-600.
Jeong YH, Yun TJ, Song JM, Park JJ, Seo DM, Koh JK, Lee SW, Kim MJ, Kang DH, Song JK. Left ventricular remodeling and change of systolic function after closure of patent ductus arteriosus in adults: device and surgical closure. Am Heart J. 2007 Sep;154(3):436-40.doi: https://doi.org/10.1016/j.ahj.2007.04.045


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


