A study of relative value of percutaneous fine needle aspiration cytology and bronchoscopy in pulmonary lesions
Abstract
Percutaneous fine needle aspiration cytology (FNAC) is a useful additional method for establishing a diagnosis of intrathoracic lesions without a thoracotomy.
Aims and Objective: To study the comparative role of FNAC. 1) In establishing the diagnosis of intrathoracic solid lesions. 2) Its role in improving the diagnostic yield.
Material and Methods: All the patients, irrespective of their age and sex, who presented with space occupying lesions in thorax, large nodular shadows and consolidation on clinico-radiological ground, were included in the study and subjected to FNAC and other procedures like fiberoptic bronchoscopy (FOB) etc.
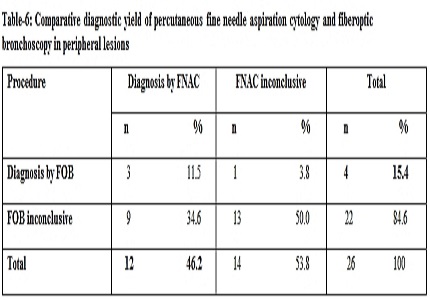
Results: 44 patients were enrolled in the study. 56.8% cases were diagnosed as primary carcinoma lung and 6.8% as benign lesions, while 36.4% cases could not be diagnosed by any means. 28 cases were diagnosed either by means of FNAC and / or by other methods of investigation like FOB and sputum cytology. Overall diagnostic yield of FNAC was 54.5%, with positivity more in central lesions (66.7%) than in peripheral lesions (46.2%). Diagnostic yield of FNAC for malignancy was 84%. Overall diagnostic yield by bronchoscopy was 17/44(38.6%). FNAC was also effective to pick up diagnosis in 13(29.5%) but failed in 4 cases which were diagnosed by bronchoscopy. Overall 6.8% patients developed minor complications.
Conclusion: Considering its simplicity, safety, rapidity, cost effective and high diagnostic accuracy FNAC can be and should be performed as an initial diagnostic measure, preceding bronchoscopy, mediastinoscopy and thoracotomy whenever exfoliative sputum cytology has failed to establish the diagnosis of the entire peripheral and selected intrathoracic lesion.
Downloads
References
Martin HE, Ellis EB. Biopsy by needle puncture and aspiration. Ann Surg. 1930 Aug;92(2):169-81.doi: https://doi.org/10.1097/00000658-193008000-00002.
Lalli AF, Naylor B, Whitehouse WM. Aspiration biopsy of thoracic lesions. Thorax. 1967;22: 404-7.doi: https://doi.org/10.1136/thx.22.5.404.
Greif J, Marmor S, Schwarz Y, Staroselsky AN. Percutaneous core needle biopsy vs. fine needle aspiration in diagnosing benign lung lesions. Acta Cytol. 1999 Sep-Oct;43(5):756-60.doi: https://doi.org/10.1159/000331287.
Wallace MJ, Krishnamurthy S, Broemeling LD, Gupta S, Ahrar K, Morello FA Jr, Hicks ME. CT-guided percutaneous fine-needle aspiration biopsy of small (< or =1-cm) pulmonary lesions. Radiology. 2002 Dec;225(3):823-8.doi: https://doi.org/10.1148/radiol.2253011465.
Chen CC, Hsu WH, Huang CM, Hsu JY, Chiang CD. Ultrasound-guided fine needle aspiration biopsy of small pulmonary nodules abutting to the chest wall. Zhonghua Yi Xue Za Zhi (Taipei). 1996 Feb;57(2):106-11.
Sarjer RN, Rabbi AF, Hossain A, Quddus MA et al. Computed tomography guided transthoracic fine needle aspiration cytology in the diagnosis of sonographically non-approachable intrathoracic masses- A study of 100 cases. J Dhaka Med Coll. 2011; 20(1): 25-31.doi: https://doi.org/10.3329/jdmc.v20i1.8568.
Fuladi AB, Munje RP, Tayade BO. Value of Washings, Brushings, and Biopsy at Fibreoptic Bronchoscopy in the Diagnosis of Lung Cancer. JIACM. 2004; 5(2): 137-42.http://medind.nic.in/jac/t04/i2/jact04i2p137.pdf.
Penketh ARL, Robinson AA, Barker V, Flower CDR. Use of percutaneous needle biopsy in the investigation of solitary pulmonary nodules. Thorax. 1987; 42: 967-71.
Johnston WW. Percutaneous fine needle aspiration biopsy of the lung. A study of 1015 patients. Acta. Cytol. 1984; 28(3):218-24.
Pavy RD, Antic R, Begley M. Percutaneous aspiration biopsy of discrete lung lesions. Cancer. 1974; 34: 2109-17.doi: https://doi.org/10.1002/1097-0142(197412)34:6%3C2109::aid-cncr2820340635%3E3.0.co;2-u.
Sarkar SK. Flexible fiberoptic bronchoscopy in the diagnosis of pulmonary pathology. J. Ind. Med. Assoc. 1983; 81(1-2): 6-9.
Gangopadhyay M, Chakrabarti I, Ghosh N, Giri A. Computed tomography guided fine needle aspiration cytology of mass lesions of lung: Our experience. Indian J Med Paediatr Oncol. 2011; 32(4): 192–6.doi: https://dx.doi.org/10.4103%2F0971-5851.95139.
Dahlgren S, Nordenström B. Transthoracic Needle Biopsy. Stockholm: Almqvist & Wiksell, 1966.doi: https://www.researchgate.net/deref/http%3A%2F%2Fdx.doi.org%2F10.1056%2FNEJM196705112761907.
Lalli AF, Mccormack LJ, Zelch M, Reich NE, Belovich D. Aspiration biopsies of chest lesions. Radiology. 1978; 127(1): 35-40.doi: https://doi.org/10.1148/127.1.35.
Jamplis RW, Stevens GM, Lillington GA. Percutaneous needle aspiration biopsy of the lung. Am. Jr. Surg. 1968; 116(2): 243-50.
Singh MM, Gupta RK, Das DK, Pant CS. Ultrasonically guided FNAC of intra thoracic lesions. Ind. Jr. Chest Dis. & All. Sci. 1987; 29(2): 81-9.
Fontana RS, Miller WE, Beubout JW. Transthoracic needle aspiration of discrete pulmonary lesions: Experience in 100 cases. Med. Clin. N. Am. 1970; 54:961-71.
Zelch JV, Lalli AF, McCormack LJ, Belovich DM. Aspiration biopsy in the diagnosis of pulmonary nodules. Chest. 1973; 63(2): 149-52.doi: https://doi.org/10.1378/chest.63.2.149.
Nordenstron BE. Technical aspect of obtaining cellular material from lesion deep in lung: A radiologists view and description of the screw needle sampling technique Acta. Cytol. 1984; 28: 233-42.
Zavela DC, Schoell JE. Ultra thin needle aspiration of the lung in infectious and malignant disease. Am. Rev. Resp. Dis. 1981; 123(1): 125-31.doi: https://doi.org/10.1164/arrd.1981.123.1.125.
Kvale PA, Bodo FR, Kini S. Diagnostic accuracy in lung cancer. Comparison of techniques used in association with flexible fiberoptic bronchoscopy. Chest. 1976; 69: 752-57.doi: https://doi.org/10.1378/chest.69.6.752.
Funahashi A, Browne TK, Houser WC, Hranicka LJ. Diagnostic value of bronchial aspirate and post bronchoscopic sputum in fiber optic bronchoscopy. Chest. 1979; 76(5): 514-7.doi: https://doi.org/10.1378/chest.76.5.514.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


