Spectrum of epilepsy in Neurocysticercosis
Abstract
Introduction: Neurocysticercosis (NCC) is one of the most common parasitic cause of neurological disease in developing countries. NCC is the infestation of the central nervous system with the larvae of pork tapeworm, Taenia solium. It is endemic in South Asia, Africa, and Latin America. Due to increasing international travel and immigration, NCC is no more a health issue limited to the developing countries but also to the rest of world.
Material and methods: A total of 70 patients of seizures presenting with ring enhancing lesion in CT scan of brain suggestive of neurocysticercosis, attending outpatient department or admitted in wards of Medicine Department of S.R.N. Hospital. A detailed seizure history as well as neurological examination was done according to the working proforma.
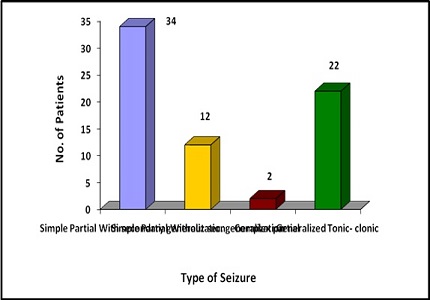
Results: Maximum number of patients 34(48.57%) were presented with simple partial seizures with secondary generalization. Generalized tonic-clonic seizure was present in 22 patient (31.43%) patients. Simple partial seizure without secondary generalization was presented in 12 patients (17.14%). Two patients (2.86%) were presented with complex partial seizure.
Conclusion: Neurocysticercosis is more common in young, rural population and in lower socioeconomic class. Vegetarians were significantly more affected than non-vegetarians which suggest other mode of transmission. By combining hygiene education and better sanitation, we will interrupt or reduce the cycle of direct person-to-person transmission. Thus, probably we will succeed to reduce the burden of disease from the society.
Downloads
References
2. White AC Jr. Neurocysticercosis: a major cause of neurological disease worldwide. Clin Infect Dis. 1997 Feb;24(2):101-13; quiz 114-5. [PubMed]
3. Recommendations of the International Task Force for Disease Eradication. MMWR Recomm Rep. 1993 Dec 31;42(RR-16):1-38. [PubMed]
4. Garcia HH, Del Brutto OH; Cysticercosis Working Group in Peru. Neurocysticercosis: updated concepts about an old disease. Lancet Neurol. 2005 Oct;4(10):653-61. [PubMed]
5. Garcia HH, Oilman RH. Cysticercosis In Oxford TextBook of Medicine 4th edition. Edited by Warrel DA, Cox TM, Firth JF. Oxford. Oxford University Press 2003; 824-829.
6. Santibanez SS, Steele RW, Mushat DM. Chronic headache in woman from Honduras. Infect Med 1999; 164:230-234.
7. Hawk MW, Shahlaie K, Kim KD, Theis JH. Neurocysticercosis: a review. Surg Neurol. 2005 Feb;63(2):123-32; discussion 132. [PubMed]
8. Jha S, Kumar V. Neurocysticercosis presenting as stroke. Neurol India. 2000 Dec;48(4):391-4.
9. Garg RK, Karak B. Neurocysticercosis presenting as midbrain syndrome. J Assoc Physicians India. 2000 May;48(5):533-5. [PubMed]
10. Singh NN, Verma R, Pankaj BK, Misra S. Neurocysticercosis presenting as Weber's syndrome. Neurol India. 2003 Dec;51(4):551-2. [PubMed]
11. Agarwal V, Kumar P, Chadda RK. Neurocysticercosis presenting as psychiatric illness. Indian J Pediatr. 2001 Nov;68(11):1073-4. [PubMed]
12. Bourgeois JA, Motosue J, Mehra N. Mood and psychotic symptoms with neurocysticercosis. Psychosomatics. 2002 Jul-Aug;43(4):337-8. [PubMed]
13. Del Brutto OH, Rajshekhar V. White Ac J. et al. Proposed diagnostic criteria for neurocysticercosis. Neurology 2001; 57:177-83. [PubMed]
14. Guidelines for epidemiologic studies on epilepsy. Commission on Epidemiology and Prognosis, International League Against Epilepsy. Epilepsia. 1993 Jul-Aug;34(4):592-6.
15. Del Brutto OH, García E, Talámas O, Sotelo J. Sex-related severity of inflammation in parenchymal brain cysticercosis. Arch Intern Med. 1988 Mar;148(3):544-6. [PubMed]
16. Banerjee P.S., Bhatia B.B. & Pandit B.A. (1994). – Sarcocystis suihominis infection in human beings in India. J. vet. Parasitol., 8 (1), 57-58.
17. Varma A, Gaur KJ. The clinical spectrum of neurocysticercosis in the Uttaranchal region. J Assoc Physicians India. 2002 Nov;50:1398-400. [PubMed]
18. Singh MK, Garg RK, Nath G, Verma DN, Misra S. Single small enhancing computed tomographic (CT) lesions in Indian patients with new-onset seizures. A prospective follow-up in 75 patients. Seizure. 2001 Dec;10(8):573-8.
19. Wadia RS, Makhale CN, Kelkar AV, Grant KB. Focal epilepsy in India with special reference to lesions showing ring or disc-like enhancement on contrast computed tomography. J Neurol Neurosurg Psychiatry. 1987 Oct;50(10):1298-301.
20. Pazzagalia B; V.Grinnel, M.A. Goldberg, and D.Heiner.1981: Spontaneous radiographic disappearance of cerebral cysticercosis. Neurology 33 : 1337-1357.
21. Kotokey RK, Lynrah KG, De A. A clinico-serological study of neurocysticercosis in patients with ring enhancing lesions in CT scan of brain. J Assoc Physicians India. 2006 May;54:366-70. [PubMed]
22. Kumar AS, Subrahmanyam DK. Neurocysticercosis presenting as pseudobulbar palsy. J Neurosci Rural Pract. 2014 Jan;5(1):76-7. doi: 10.4103/0976-3147.127883. [PubMed]
23. Del Brutto OH, Sotelo J, Aguirre R, Díaz-Calderón E, Alarcón TA. Albendazole therapy for giant subarachnoid cysticerci. Arch Neurol. 1992 May;49(5):535-8.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


