Changing epidemiology of poisoning in Central India: shifting poles from male farmers to young house wives
Abstract
Introduction: Acute self infliction of poisoning is very common among young in developing countries. The epidemiology of poisoning changes time to time and varies region to region. In south India, organophosphorus compound poisoning has been more common as compared to Aluminium phosphide poisoning in north India. All over India males are more commonly reported to poison themselves. Poisoning in farmers has been reported more commonly than in any other profession. Madhya Pradesh is situated in central part of India, where agriculture is the predominant source of income. There is a knowledge gap in epidemiology of poisoning in this region.
Methods: This is a hospital based observational type cross sectional study over nearly 2 years.
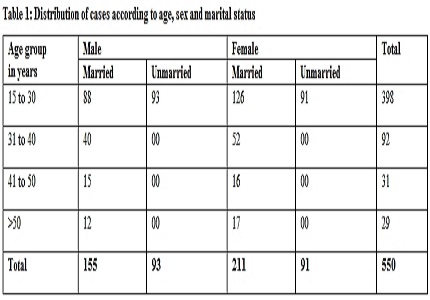
Results: Out of the 550 number of study participants about 90% were younger than 40 years. Females were more common than males in all age groups. Poisoning was more common in married population in both the genders. House wives followed by unemployed students were the most vulnerable populations. Farmers constituted only about 10% of total cases. Organophosphorus compounds were the most common type of poisoning contributing to almost one fourth of the total cases followed by Zinc phosphide, Aluminium phosphide, oleander and ethylene dibromide poisoning in decreasing order. The overall mortality was 9.8% (n=54). The case fatality rates of various agro-chemicals in decreasing order were Aluminum phosphide (44.7%), ethylene dibromide (17.6%), and organophosphorus (7%). These 3 poisonings contributed to 92.5% of all deaths. Death was more common when the time lag to hospitalization was > 6 hours.
Conclusion: Younger age group, female sex and housewives were the most vulnerable group. The case fatality rate of various poisonings in decreasing order were Aluminum phosphide (Celphos) poisoning followed by EDB and OPC.
Downloads
References
2. Sharma BR, Harish D, Sharma V, Vij K. Poisoning in northern India: changing trends, causes and prevention thereof. Medicine, science and the law. 2002 Jul 1;42(3):251-7. [PubMed]
3. Evans GJ. Deliberate self-poisoning in Oxford area. Br J Prev Soc Med. 1967;21:97–107. [PubMed]
4. Smith AJ. Self- poisoning with drugs: A worsening situation. Br Med J. 1972;4:57–9. [PubMed]
5. Rygnestad T. A comparative prospective study of self-poisoned patients in Trondheim, Norway between 1978 and 1987: Epidemiology and clinical data. Hum Toxicol. 1989;8:75–82. [PubMed]
6. World Health Organisation Bulletin (1999): Guidelines for Poison Control, WHO, Geneva. [PubMed]
7. Taruni NG, Bijoy TH, Momonchand A. A profile of poisoning cases admitted in RIMS Hospital, Imphal. Journal of Forensic Medicine and Toxicology. 2001;18(1):31-3.
8. Pillay V.V. In: MKR Krishna’s Hand Book of Forensic Medicine and Toxicology, 12th Ed., Paras Publications, Hyderabad,2001: p 276-299.
9. Eddleston M. Patterns and problems of deliberate self‐poisoning in the developing world. Qjm. 2000 Nov 1;93(11):715-31. [PubMed]
10. Batra AK, Keoliya AN, Jadhav GU. Poisoning: an unnatural cause of morbidity and mortality in rural India. Journal-Association of Physicians of India. 2003 Oct 1;51:955-9. [PubMed]
11. Mannaim PF. Pattern of acute intoxication in Florence: A comparative investigation. Intensive Care Med. 1991; 17(1): 24-31. [PubMed]
12. Begum JA, Chowdhury MM. G Ara. A study of poisoning cases in four hospitals of Bangladesh Bangladesh Med J. 1989; 18(2): 64. [PubMed]
13. Siwach SB, Gupta A. The profile of acute poisoning in Haryana. J Assoc Physicians India.1995;13:756–9. [PubMed]
16. Kanchan T,Menzes RG.Suicidal poisoning in Southern India:Gender differences.J Forensic Leg Med 2008;15;7-14. [PubMed]
17. Singh B, Unnikrishnan B. A profile of acute poisoning at Mangalore (South India). J Clin Forensic Med 2006;13:112-6. [PubMed]
18. Nigam M, Jain AK, Dubey BP, Sharma VK. Trends of organophosphorus poisoning in bhopal region an autopsy based study. JIAFM 2004;26:971-3.
19. Kumar SV, Venkateswarlu B, Sasikala M, Kumar GV. A study on poisoning cases in a tertiary care hospital. J Nat Sci Biol Med. 2010;1:35–9. [PubMed]
20. Eddleston M. Patterns and problems of deliberate self‐poisoning in the developing world. Qjm. 2000 Nov 1;93(11):715-31. [PubMed]
21. Zamani J, Aslani A. Cardiac findings in acute yellow oleander poisoning. Journal of cardiovascular disease research. 2010 Mar 31;1(1):27-9.
22. Tufekci IB, Curgunlu A, Sirin F. Characteristics of acute adult poisoning cases admitted to a university hospital in Istanbul. Hum Exp Toxicol. 2004;23:347–51. [PubMed]
23. Yamashita M, Matsuo H, Tanaka J. Analysis of 1000 consecutive cases of acute poisoning in the suburb of Tokyo leading to hospitalization. Vet Hum Toxicol. 1996;38:34–5. [PubMed]
24. Singh S, Sharma BK, Wahi PL. Spectrum of acute poisoning in adults (10 years experience) J Assoc Physicians India. 1984;32:561–3. [PubMed]
25. Singh S, Wig N, Chaudhary D, Sood N, Sharma B. Changing pattern of acute poisoning in adults: Experience of a large North West Indian hospital (1970–1989) J Assoc Physicians India. 1997;45(3):194–7. [PubMed]
26. Van der Hoek W. Analysis of 8000 hospital admissions for acute poisoning in a rural area of Sri Lanka. Clinical Toxicology. 2006 Jan 1;44(3):225-31.
27. Rajasuriar R, Awang R, Hashim SB, Rahmat HR. Profile of poisoning admissions in Malaysia. Hum Exp Toxicol 2007;26:73-81. [PubMed]
28. Mohanty MK, Kumar V, Bastia BK, Arun M. An analysis of poisoning deaths in Manipal, India. Vet Hum Toxicol 2004;46:208-9. [PubMed]
29. Ahmad M, Rahman FN, Ashrafuzzaman M, Chowdhury DK, Ali M. Overview of Organo-phosphorus Compound Poisoning in Bangladesh and Medico-legal Aspects Related to Fatal Cases. Journal of Armed Forces Medical College, Bangladesh. 2009;5(1):41-5.
30. Gupta S, Kumar S, Sheikh MI. Comparative study and changing trends of poisoning in year 2004–2005, at Surat, India. International Journal of Medical Toxicology & Legal Medicine. 2007;10(1):16-20.
31. Murali R, Bhalla A, Singh D, Singh S. Acute pesticide poisoning: 15 years experience of a large North-West Indian hospital. Clinical toxicology. 2009 Jan 1;47(1):35-8.
32. Thapa SR, Lama P, Karki N, Khadka SB. Pattern of poisoning cases in Emergency Department of Kathmandu Medical College Teaching Hospital. Kathmandu University medical journal (KUMJ). 2007 Dec;6(2):209-13.
33. Sheu JJ, Wang JD, Wu YK. Determinants of lethality from suicidal pesticide poisoning in metropolitan HsinChu. Vet Hum Toxicol 1998; 40:332–6. [PubMed]
34. Louriz M, Dendane T, Abidi K, Madani N, Abouqal R, Zeggwagh AA. Prognostic factors of acute aluminum phosphide poisoning. Indian journal of medical sciences. 2009 Jun 1;63(6):227. [PubMed]
35. Mathai A, Bhanu MS. Acute aluminium phosphide poisoning: Can we predict mortality?. Indian journal of anaesthesia. 2010 Jul 1;54(4):302. [PubMed]
36. Nigam M, Godaria I, Varma A, Chaturvedi R. Ethylene di-bromide (EDB)–An underestimated lethal pesticide and its emerging clinico-biochemical trends. Medico-Legal Update. 2010;10(2). [PubMed]
37. Adlakha A, Philip PJ, Dhar KL. Organophosphorus and carbamate poisoning in Punjab. The Journal of the Association of Physicians of India. 1988 Mar;36(3):210. [PubMed]
38. Uma.M.A. et al :Correlation of serum cholinesterase ;clinical score at presentation & severity of organophosphorus compound poisoning MD Thesis ,RGUHS ,2011 Karnatka.
39. Arup KK. Predictors of mortality in organophosphorus poisoning–Hospital based study from suburban West Bengal. J Assoc Physicians India. 2011 Jan;49:91.
40. Ram JS, Kumar SS, Jayarajan A, Kuppuswamy G. Continuous infusion of high doses of atropine in the management of organophosphorus compound poisoning. The Journal of the Association of Physicians of India. 1991 Feb;39(2):190-3.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


