A prospective, randomized, double blind controlled trial of the use of preoperative antibiotics in routine abdominal surgery: A comparative analysis between Ofloxacin + Metronidazole, Cefotaxime + Sulbactum and Cefepime +Tazobactum (Single does vs. Three
Abstract
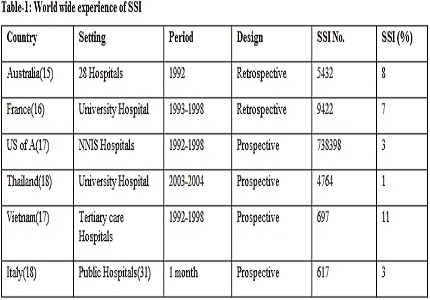
Introduction: Anti microbial prophylaxis before any elective surgery is a preferred deterrent to post operative surgical site infection now. We have used different antibiotics, two being from the cephalosporin class, one from the fluoroxoqiuinolones and anti beta lactamases in combination along with metronidazole. The aim was to find out the best and most economical pre operative prophylaxis in our surgical practice. Three antibiotics regimens were studied. Patients were divided into two groups against each agent of Ofloxacin +Metronidazole, Cefotaxime + Sulbactum and Cefepime +Tazobactum. They were again subdivided into two groups one receiving single dose and another three doses of the antibiotics regimens.
Methods: A total of 138 patients (above 16 years) were taken for the study. It was a randomized and blind study. Patients were prospectively analysed. First, the patients were divided into two groups. First group received a single dose of antibiotic at incision and those who received two more doses at eight hours interval after the dose at incision.
Discussion: The single dose pre operative prophylaxis scored over three doses regime in all the cases for lap surgery irrespective of OT condition. Three doses regime worked better in combined OT condition for the open elective procedures. The study also revealed the most economic choice for routine elective abdominal surgery.
Conclusion: Multiday and antibiotics use for a prolonged period is not advisable these days after a routine elective abdominal surgery. Single dose injection of antibiotics at a proper time is good enough for preventing postoperative surgical site infection after a routine Laparoscopic surgery. Three doses regime is better in open surgical cases performed in OTs where emergency procedures are undertaken. It is advisable to use the most cost effective regime to reduce the healthcare cost in the country.
Downloads
References
2. Auerbach AD. Prevention of Surgical Site infection. Agency for healthcare Research and Quality 2001:221-44
3. Nigel Mark Bagnall et al. Surgical site infection. Surgery October 2009,Volume 27, Issue 10, Pages 426–430 DOI: http://dx.doi.org/10.1016/j.mpsur.2009.08.007
4. Mangram AJ et al. Guideline for prevention of Surgical site infection, Infect Control Hosp Epidemiol 199;20:247-80
5. Mandell GL et al,Douglas and Bennett’s Principles and practice of infectious diseases. 6th. EditionNew York:Elsevier/Churchill Livingstone, 2005
6. Dellinger EP et al, Quality standard for antimicrobial prophylaxis in surgical procedures. Infectious diseases society of America. Clinical infectious disease, 1994;18:422-27
7. McManus AT, Solomkin JS, Wittmann DH. Antimicrobial prophylaxis for surgical wounds. Guidelines for clinical care. Arch Surg. 1993 Jan;128(1):79-88.
8. Meijer WS, Schmitz P et al. Meta analysis ofRandomized controlled clical trials of antibiotics prophylaxis in biliary tract surgery. British Journal of Surgery 1990; 77: 283-90
9. DiPiro JT, Cheung RP, Bowden TA Jr, Mansberger JA. Single dose systemic antibiotic prophylaxis of surgical wound infections. Am J Surg. 1986 Nov;152(5):552-9.
10. Platell C, Hall JC. The prevention of wound infection in patients undergoing colorectal surgery. J Hosp Infect. 2001 Dec;49(4):233-8.
11. Dimick JB, Chen SL, Taheri PA, Henderson WG, Khuri SF, Campbell DA Jr. Hospital costs associated with surgical complications: a report from the private-sector National SurgicalQuality Improvement Program. J Am Coll Surg. 2004 Oct;199(4):531-7.
12. Kirkland KB, Briggs JP, Trivette SL, Wilkinson WE, Sexton DJ. The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs. Infect Control Hosp Epidemiol. 1999 Nov;20(11):725-30.
13. Fiona Burton. Preventing surgical site infections. Wound essentials 2007;2:124-31
14. Coello R, Charlett A, Wilson J, Ward V, Pearson A, Borriello P. Adverse impact of surgical site infections in English hospitals. J Hosp Infect. 2005 Jun;60(2):93-103.
15. Kable AK, Gibberd RW, Spigelman AD. Adverse events in surgical patients in Australia. Int J Qual Health Care. 2002 Aug;14(4):269-76.
16. Rioux C, Grandbastien B, Astagneau P. The standardized incidence ratio as a reliable tool for surgical site infection surveillance. Infect Control Hosp Epidemiol. 2006 Aug;27(8):817-24. Epub 2006 Jul 24.
17. Nguyen D, MacLeod WB, Phung DC, Cong QT, Nguy VH, Van Nguyen H, Hamer DH. Incidence and predictors of surgical-site infections in Vietnam. Infect Control Hosp Epidemiol. 2001 Aug;22(8):485-92.
18. Moro ML, Morsillo F, Tangenti M, Mongardi M, Pirazzini MC, Ragni P; ICN Regional Group. Rates of surgical-site infection: an international comparison. Infect Control Hosp Epidemiol. 2005 May;26(5):442-8.
19. Freeman CD, Klutman NE, Lamp KC. Metronidazole. A therapeutic review and update. Drugs. 1997 Nov;54(5):679-708.
20. Karchmer, A.W. Cephalosporins. In, Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases, 5th ed. (Mandell, G.L., Bennett, J.E., and Dolin, R., eds.) Churchill Livingstone, Philadelphia, 2000, pp. 274-291.
21. Bryson HM, Brogden RN. Piperacillin/tazobactam. A review of its antibacterial activity, pharmacokinetic properties and therapeutic potential. Drugs. 1994 Mar;47(3):506-35.
22. Eliopoulos, G.M., and Eliopoulos, C.T. Activity in vitro of the quinolones. In, Quinolone Antimicrobial Agents, 2d ed. (Hooper, D.C., and Wolfson, J.S., eds.) American Society for Microbiology, Washington, 1993, pp. 161-193.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


