To study the clinicobacteriological profile and antibiotic susceptibility pattern of community acquired pyodermas
Abstract
Background: Pyodermas are the pyogenic skin infection encountered in dermatologic clinic and is mainly caused by Staphylococci and Streptococci.
Aim: To find out causative organisms in community acquired pyodermas and their current antibiotic susceptibility patterns.
Materials and Methods: All the patients attending the Dermatology OPD in Government Medical College, Amritsar were screened over 18 months and swabs were sent for culture and sensitivity.
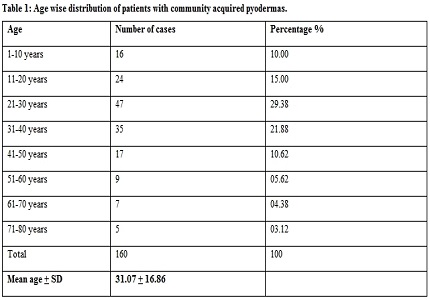
Results: The maximum incidence of pyodermas was observed in patients of 21-40 years i.e 82(51.24%). Most of the patients were males i.e 95(64%) than females i.e 64(40%). Out of 160 patients, maximum patients i.e. 109(68.13%) had secondary pyoderma and 51 (31.87%) had primary pyodermas. Out of 160 samples, growth was obtained in 148 (92.50%) samples while 12(07.50%) samples showed no growth. Most common organisms isolated was Staphylococcus aureus in 70 (43.75%) cases followed by CONS in 20(12.50%) cases. Among the Gram negative organisms E.coli was observed to be the common isolate in 16(10.00%) cases followed by Pseudomonas aeruginosa in 12(07.50%) cases. On antibiotic susceptibility testing, Gram positive organisms, maximum sensitivity i.e 100% was seen to vancomycin, linezolid and maximum resistance i.e 84.29% was seen to ampicillin. Among the Gram negative isolates maximum sensitivity i.e 100% was seen to Imipenem, Piperacillin -Tazobactum and Sulbactam-Ceftazidime and maximum resistance i.e 100% was seen to ceftazidime in case of Acinetobacter.
Conclusion: This study gives an indication of the present pattern of bacteriological profile and antibiotic susceptibility pattern of pyodermas in a tertiary care hospital in north India.
Downloads
References
2. Gandhi S, Ojha AK, Ranjan KP, Neelima. Clinical and bacteriological aspects of pyoderma. N Am J Med Sci. 2012 Oct;4(10):492-5. doi: 10.4103/1947-2714.101997. [PubMed]
3. Paudel U, Parajuli S, Pokhrel DB. Clinico-bacteriological profile and antibiotic susceptibility pattern in pyodermas: A hospital based study.Nep J Dermatol Venereol Leprol. 2013;11(1):49-57.
4. Nagmoti JM, Patil CS, Metgud SC. A bacterial study of pyoderma in Belgaum. Indian J Dermatol Venereol Leprol. 1999 Mar-Apr;65(2):69-71. [PubMed]
5. Ramani TV and Jayakar PA: Bacteriological study of 100 cases of Pyodermas with special reference to Staphylococci, antibiotic sensitivity and phage pattern. Ind J Dermatol Venereol Leprol. 1980;46(5):282-286. [PubMed]
6. Tan Hiok Hee. A study of bacterial skin infection in NSC. NSC Bulletin for Medical Practitioners. 1996;7(2).
7. Ayyagari A, Agarwal KC, Kaur S, Iyer RV, Kumar B. Prevalence of Corynebacterium diphtheriae in pyoderma and other skin lesions. ndian J Pathol Microbiol. 1979 Jan;22(1):37-45. [PubMed]
8. Clinical Laboratories Standard Institute. Performance standards for antimicrobial disks susceptibility tests. Approved standards, 11th ed. CLSI document M2-A12. CLSI,
Wayne, PA: CLSI 2012. [PubMed]
9. Park K. Health information and basic medical statistics. In: Park K, Park’s textbook of preventive and social medicine. 21st ed. Bansari das Bhanot, India; 2011.p.779-92. [PubMed]
10. Kharel C, Pandey SS, Agrawal S, Khanal B. Clinico-bacteriological study of pyoderma in children. Nep J Dermatol Venereol Leprol. 2012;10(1):11-5.
11. Janardhan. B, Prasad.G K, Nandeshwar AJ and Vidyavathi N. Clinico-microbiological study of pyodermas. International Journal of Recent Scientific Research. 2015;6(5):3820-3824.
12. Mathews MS, Garg BR, Kanungo R. A clinico-bacteriological study of primary pyodermas in children in Pondicherry. Ind J Dermatol Venereol Leprol. 1992;58(3):183-7.
13. Neirita Hazarika A Clinico-Epidemiological Study of Pyoderma in Children. Nat.J.Res.Com.Med. 2012;1(4):178 -241.
14. Malhotra SK, Malhotra S, Dhaliwal GS, Thakur A. Bacteriological study of pyodermas in a tertiary care dermatological center. Indian J Dermatol. 2012 Sep;57(5):358-61. doi: 10.4103/0019-5154.100475.
15. Sonaiya T, Javedkar T, Patel S, Kinariwala D, Govind N. Clinico-bacteriological study of pyoderma with special reference to community acquired methicillin resistant Staphylococcus aureus. Nat J Int Res Med. 2012;3(1):21-5.
16. Sanjiv Choudhary, Taru Aghi, Shilpi Basak, and Adarshlata Singh Clinico-Bacteriological Study of Pyoderma with Special Reference to Antibiotic Sensitivity in a Tertiary Care Rural Hospital. RJPBCS. 2015;6(2):1701.
17. Janardhan. B, Prasad.G K, Nandeshwar AJ and Vidyavathi N. Clinico-microbiological study of pyodermas. International Journal of Recent Scientific Research Research. 2015;6(5):3820-3824.
18. Patil R, Baveja S, Nataraj G, Khopkar U. Prevalence of methicillin-resistant Staphylococcus aureus (MRSA) in community-acquired primary pyoderma. Indian J Dermatol Venereol Leprol. 2006 Mar-Apr;72(2):126-8.
19. Mohanty S, Kapil A, Dhawan B, Das BK. Bacteriological and antimicrobial susceptibility profile of soft tissue infections from Northern India. Indian J Med Sci. 2004 Jan;58(1):10-5.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


