Lymphovascular malformations, imaging spectrum on USG and CT (with emphasis on intralesional haemorrhage) - A descriptive study
Abstract
Introduction- Lymph vascular/lymphatic malformations usually affect infants or children. Most common sites are the head and neck. When, superficial, they present with growing swelling in affected part. Their preoperative evaluation is necessary for better postoperative outcome and to reduce the chances of recurrence. Ultrasound is the useful modality to depict the exact location and character of lesion. Colour Doppler demonstrates vascular nature of lesions. CECT providing three dimensional views of lesion as well as insinuation/extension in adjacent structures, ensuring complete surgical removal of lesion and better postoperative outcome. Method –We studied imaging spectrum of LVMs (lymphovascular malformations) in USG and colour Doppler in 40 patients at Gandhi medical college Bhopal.29 patients have further undergone CECT for better depiction of lesion. We noted imaging spectrum of lesions on USG and CECT.
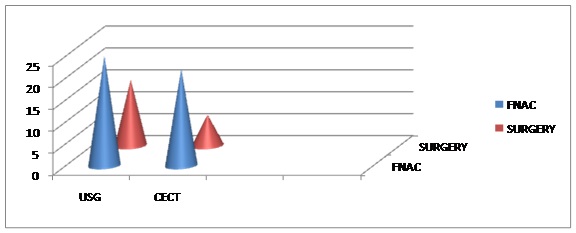
Results-Most patients presenting with growing/congenital swelling were infants. Most common finding in USG was complex multisptated cystic lesion showing intraseptal vascularity on Doppler CECT demonstrated multiseptated cystic lesion with peripheral and septal enhancement. Most of them were fluid density lesion and showing insinuation in adjacent structure.18 patients were confirmed on FNAC and 22 patients were confirmed on surgery.
Conclusion-USG is best mean to describe the character and location of lesion, also widely available, easy to use and suitable for infants and children (no sedation required). Many cases require further imaging with CECT, for further characterization of lesion and to evaluate their extension/insinuation. Surgical removal is final treatment keeping the incidences of recurrences low.
Downloads
References
2. Mandel L. Parotid area lymphangiomas in an adult: case report. J Oral Maxillofac Surg.2004; 62(10):1320–1323. doi: 10.1016/j.joms.2003.12.040.
3. Bailey CM. Cystic hygroma. Lancet. 1990; 335:511–512. doi: 10.1016/0140- 6736(90)92683-9.
4. Iyer R, Eftekhari F, Varma D, Jaffe N. Cystic retroperitoneal lymphangioma: CT, ultrasound and MR findings.Pediatr Radiol. 1993; 23(4):305-6.
5. Machado LE, Osborne NG, Bonilla-Musoles F. Three-dimensional sonographic diagnosis of lymphangiomas. J Ultrasound Med. 2004; 23(6):877–881.
6. Kraus R, Han BK, Babcock DS, Oestreich AE. Sonography of neck masses in children.AJR 1986, 146:609-613.
7a. Davidson AJ, Hartman DS. Lymphangioma of the retroperitoneum:CT and Sonographic characteristics Radiology. 1990 May; 175(2):507-10
7b. Buckmiller LM, Richter GT, Suen JY. Diagnosis and management of hemangiomas and vascular malformations of the head and neck. Oral Dis. 2010;16:405–418. [PubMed]
8. Lugo-Olivier CH, Taylor GA. CT differentiation of large abdominal lymphangioma from ascites. PediatrRadiol 1993; 23:129–130
9. Mandel L. Parotid area lymphangiomas in an adult: case report. J Oral Maxillofac Surg.2004; 62(10):1320–1323. doi: 10.1016/j.joms.2003.12.040.
10. Toranzo JM, Guerrero F, et al. A congenital neck mass. Oral Surg Oral Med Oral Pathol.1996;82(4):363–364. [PubMed]
11. Osborne TE, Alex Haller J, et al. Submandibular cystic hygroma resembling a plunging ranula in a neonate—review and report of a case. Oral Surg Oral Med Oral Pathol. 1991;71(1):16–20. Doi: 10.1016/0030-4220(91)90513-C. [PubMed]
12. Saijo M, Munro IR, Mancer K. Lymphangioma—a long term follow-up study. Plast Reconstr Surg.1975; 56:642–651. doi: 10.1097/00006534-197511000-00006. [PubMed]
13. Fraser SE, Campbell B, et al. Pathologic quiz 2. Arch Otolaryngol Head Neck Surg. 1996; 122:1200. [PubMed]
14. Hudson JW, Meszaros EJ. Submucosal lymphangiomas of the maxillary sinus. J Oral and Maxillofacial Surgery. 2003; 61: 390–392. [PubMed]
15. Roisman I, Manny J, Fields S, Shiloni E. Intra-abdominal lymphangioma. Br J Surg. 1989; 76:485–489. [PubMed]
16. Hardin WJ, Hardy JD. Mesenteric cysts. Is J Surg. 1970; 119:640–645. [PubMed]
17. Daniel S, Lazarevic B, Attia A. Lymphangioma of the mesentery of the jejunum: report of a case and a brief review of the literature. Am J Gastroenterol. 1983; 78:726–729. [PubMed]
18. Rieker RJ, Quentmeier A, Weiss C, Kretzschmar U, Amann K, Mechtersheimer G, Bläker H, Herwart OF. Cystic lymphangioma of the small-bowel mesentery: case report and a review of the literature. Pathol Oncol Res. 2000;6:146–148.
19. Sheth S, Nussbaum AR, Hutchins GM, Sanders RC. Cystic hygromas in children. Sonographic pathologic correlation, Radiology 1987, 162:821-824.
20. Serres MD, Sie KCY, et al. Lymphatic malformations of the head and neck: proposal for staging. Arch Otolaryngol Head Neck Surg. 1995; 121(5):577–582. [PubMed]
21. Goodman P, Yeung CS, Batsakis JG. Retropharyngeal lymphangioma presenting in an adult.Otolaryngol Head Neck Surg. 1990; 103(3):476–479. [PubMed]
22.S chefter RP, Olsen KD, Gaffey TA. Cervical lymphangioma in the adult. Otolaryngol Head Neck Surg.1985; 93(1):65–69. [PubMed]
23. Muñoz Herrera A, Pérez Plasencia D, Gómez Benito M, Santa Cruz Ruiz S, Flores Corral T, Aguirre García F. Cervical lymphangioma in adults- Description of 2 cases. Ann Otolaryngol Chir Cervicofac.1998; 115(5):299–302.
24. Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: a new classification based on endothelial characteristics. Plast Reconstr Surg. 1982; 69:412–422. doi: 10.1097/00006534-198203000-00002.
25. Jackson IT, Carreno R, et al. Haemangioma, lymphatic malformations and lymphovenous malformations: classification and methods of treatment. Plast Reconstr Surg. 1993; 91(7):1216–1230. doi: 10.1097/00006534-199306000-00006.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


