Differences Between Premenopausal And Postmenopausal Coronary Artery Disease (CAD) Risk Factors and Clinical Profile
Abstract
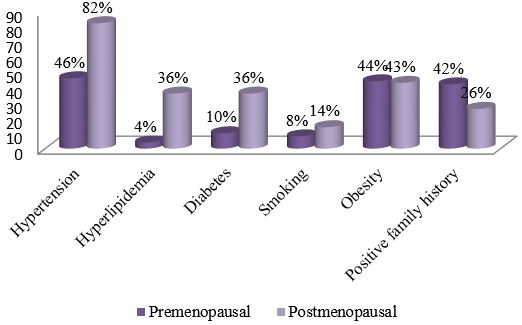
Introduction: Coronary artery disease is the leading cause of mortality and morbidity of both men and women accounting for over one third of total deaths [1]. It has reached epidemic proportion among Indians. It accounts for 1 out of 3 women death regardless of the race or ethnicity [2]. In women, the annual mortality rate from CAD is high. Objective: To assess the differences between premenopausal and postmenopausal coronary artery disease (CAD) risk factors, clinical manifestation, clinical profile and angiographic characteristics. Methods: A prospective observation study was conducted at cardiology department, NICVD, Dhaka, Bangladesh from January to December 2019. Total 200 female CAD patients were drawn from the cardiology department. The subjects were enrolled in accordance with the criterion of diameter stenosis ≥50% in left mean and ≥70% in LAD, LCX and ECA in at least one invasive coronary angiogram. Patients with pulmonary embolism, aortic aneurysm, congenital heart disease, rheumatic heart disease, myocarditis, or cardiomyopathy were excluded. A total of 50 premenopausal cases and 150 postmenopausal cases were enrolled according to their status at the time of diagnosis. All patients underwent percutaneous coronary intervention and were given conventional drug therapy for coronary artery disease during follow-up. Results: Differences were compared between the 2 groups. Fewer premenopausal women suffered from hypertension (46% versus 82%, P< 0.001), type 2 diabetes (10% versus 36%, P = 0.001), and hyperlipidemia (4% versus 36%, P<0.001), but more had a positive family history of premature CAD (42% versus 26%, P = 0.03). Acute coronary syndrome (ACS) was more frequently seen in premenopausal women (80% versus 48%, P < 0.001), and their left anterior descending branch was the vessel most often involved (68%). The cumulative recurrence rate was 1.76 times higher in postmenopausal patients than premenopausal patients. Clinical diagnosis (HR = 2.54, 95%CI: 1.21-4.85, P = 0.02) and type 2 diabetes (HR = 4.10, 95%CI: 2.37-8.83, P = 0.004) were two factors that influenced recurrence in premenopausal subjects, while the clinical diagnosis (HR = 1.93, 95%CI: 1.59-3.46, P = 0.03) and Gensini score (HR =1.20, 95% CI: 1.11-1.45, P = 0.02) were influencing factors in the postmenopausal patients. Symptoms among younger women were atypical, but the onset of disease was faster and more urgent. Conclusion: Our study clarified the differences between postmenopausal and premenopausal women with respect to risk factors, clinical symptoms, cardiovascular features, and recurrence rate, and provided a reference for further study on the mechanism and prognosis in postmenopausal or premenopausal CAD patients.
Downloads
References
2. Thom T., Hasse N., Rosamond W. Heart disease and stroke statistics-2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006;113: e85.
3. Yusuf S., Hawken S., Ounpuu S. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004; 364:937.
4. Bangladesh Bureau of Statistics. Health, family planning & social statistics. BBS, Dhaka. 2006; Tab. no. 13-20.
5. Gupta R.V. Trends in hypertension epidemiology in India. J Hum Hypertens. 2004; 18:73–78.
6. Prabhakaran D., Chaturvedi V., Shah P. Differences in the prevalence of metabolic syndrome in urban and rural India: a problem of urbanization. Chronic Illn. 2007; 3:8–19.
7. Reddy KS, Yusuf S. Emerging epidemic of cardiovascular disease in developing countries. Circulation. 1998; 97:596-601.
8. 5. Nair M, Prabhakaran D. Why do South Asians have high risk for CAD? Global Heart. 2012; 7:307-14.
9. Solimene MC. Coronary heart disease in women: a challenge for the 21st century. Clinics 2010; 65:99-106.
10. 2. Mosca L, Benjamin EJ, Berra K, Bezanson JL, Dolor RJ, Lloyd-Jones DM, et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women—2011 update: a guideline from the American Heart Association. Circulation 2011;123: 1243–62
11. Leifheit‑ Limson EC, D’Onofrio G, Daneshvar M, Geda M, Bueno H, Spertus JA, et al. Sex differences in cardiac risk factors, perceived risk, and health care provider discussion of risk and risk modification among young patients with acute myocardial infarction: The VIRGO study. J Am Coll Cardiol 2015; 66:1949‑ 57.
12. Bettegowda S. Clinical profile of ischemic heart disease in women with special reference to the risk factors. Sch J App Med Sci 2014; 2:3020‑ 5.
13. Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case‑ control study. Lancet 2004; 364:937‑ 52.
14. Oomman A, Sathyamurthy I, Ramachandran P, Verghese S, Subramanyan K, Kalarickal MS, et al. Profile Of female patients undergoing coronary angiogram at a tertiary centre. J Assoc Physicians India 2003; 51:16‑ 9.
15. Wenger NK. Coronary heart disease: The female heart is vulnerable. Prog Cardiovasc Dis 2003; 46:199‑ 229.
Copyright (c) 2024 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


