Antimicrobial Resistance and its Impact on Public Health
Abstract
Aim of the Study: The current study addresses the increasing threat of AMR and its direct impact on global public health. It aims to contribute to the existing knowledge about the key challenges of AMR, bringing attention to the need for further research and creating a combined effort in the battle with antimicrobial resistance.
Background & Methods: Antimicrobial resistance (AMR) has been considered one of the key problems that humankind has come across, showing a massive impact on public health globally. The continuous emergence of new microbial strains complicates it further by reducing the efficacy of the available antimicrobial drugs. For the current study, various scientific journals were studied from multiple resources. Furthermore, the websites of policymakers and agencies associated with this cause were studied and referred to.
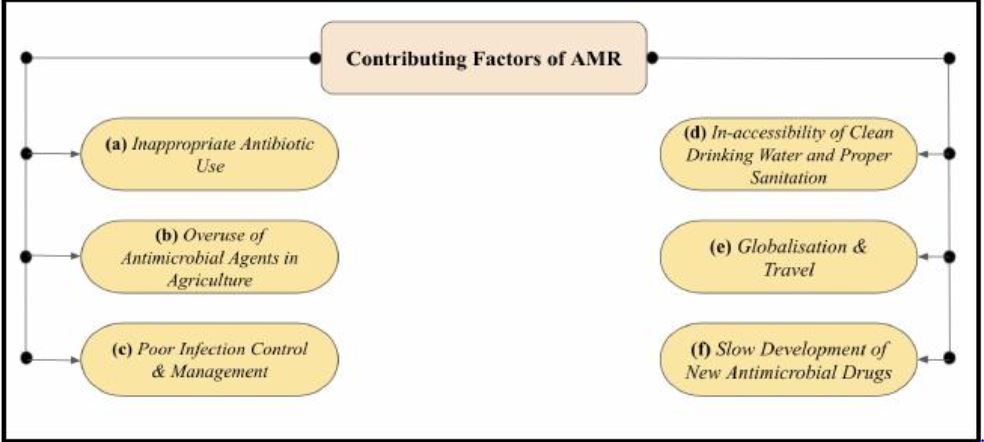
Results & Conclusions: The study has revealed a concerning trend of a steep increase in resistance of pathogens to antimicrobial agents. The major contributing factors which were identified during this study include misuse and overuse in the healthcare sector, inadequate prevention of infections and disease control, overuse in agriculture and the lack of novel antimicrobial agents. Several policies like the “One Health” approach by the Centers for Disease Control and Prevention (CDC) and the United Nations Sustainable Development Goals (SDGs) have been put in place as a means to combat the global public health problem. The study also highlights the need for policymakers, stakeholders and researchers to work in unison to combat the global issue.
Downloads
References
Ferri, M., Ranucci, E., Romagnoli, P., & Giaccone, V. (2017). Antimicrobial resistance: A global emerging threat to public health systems. Critical reviews in food science and nutrition, 57(13), 2857-2876.
Giaccone, G., & Pinedo, H. M. (1996). Drug resistance. The oncologist, 1(1-2), 82-87.
Ribeiro da Cunha, B., Fonseca, L. P., & Calado, C. R. (2019). Antibiotic discovery: where have we come from, where do we go?. Antibiotics, 8(2), 45.
Antibiotic Resistance. World Health Organisation. Retrieved April 11, 2024, from https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance#:~:text=It%20is%20estimated%20that%20bacterial,development%20of%20drug%2Dresistant%20pathogens.
Murray, C. J., Ikuta, K. S., Sharara, F., Swetschinski, L., Aguilar, G. R., Gray, A., ... & Tasak, N. (2022). Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. The lancet, 399(10325), 629-655.
JJonas, O. B., Irwin, A., Berthe, F. C. J., Le Gall, F. G., & Marquez, P. V. (2017). Drug-resistant infections: a threat to our economic future. Washington, DC: World Bank Group.
Llor, C., & Bjerrum, L. (2014). Antimicrobial resistance: risk associated with antibiotic overuse and initiatives to reduce the problem. Therapeutic advances in drug safety, 5(6), 229-241.
Sekyere, J. O., & Asante, J. (2018). Emerging mechanisms of antimicrobial resistance in bacteria and fungi: advances in the era of genomics. Future microbiology, 13(2), 241-262.
Kariyawasam, R. M., Julien, D. A., Jelinski, D. C., Larose, S. L., Rennert-May, E., Conly, J. M., ... & Barkema, H. W. (2022). Antimicrobial resistance (AMR) in COVID-19 patients: a systematic review and meta-analysis (November 2019–June 2021). Antimicrobial Resistance & Infection Control, 11(1), 45.
Lipsitch, M., Singer, R. S., & Levin, B. R. (2002). Antibiotics in agriculture: when is it time to close the barn door?. Proceedings of the National Academy of Sciences, 99(9), 5752-5754.
Woodford, N., & Ellington, M. J. (2007). The emergence of antibiotic resistance by mutation. Clinical Microbiology and Infection, 13(1), 5-18.
Bush, K., & Bradford, P. A. (2016). β-Lactams and β-lactamase inhibitors: an overview. Cold Spring Harbor perspectives in medicine, 6(8), a025247.
Soucy, S. M., Huang, J., & Gogarten, J. P. (2015). Horizontal gene transfer: building the web of life. Nature Reviews Genetics, 16(8), 472-482.
Boto, L. (2010). Horizontal gene transfer in evolution: facts and challenges. Proceedings of the Royal Society B: Biological Sciences, 277(1683), 819-827.
Abebe, E., Tegegne, B., & Tibebu, S. (2016). A review on molecular mechanisms of bacterial resistance to antibiotics. European Journal of Applied Sciences, 8(5), 301-310.
Cloete, T. E. (2003). Resistance mechanisms of bacteria to antimicrobial compounds. International Biodeterioration & Biodegradation, 51(4), 277-282.
Baquero, F., Alvarez‐Ortega, C., & Martinez, J. L. (2009). Ecology and evolution of antibiotic resistance. Environmental Microbiology Reports, 1(6), 469-476.
Zhang, L., Levy, K., Trueba, G., Cevallos, W., Trostle, J., Foxman, B., ... & Eisenberg, J. N. (2015). Effects of selection pressure and genetic association on the relationship between antibiotic resistance and virulence in Escherichia coli. Antimicrobial agents and chemotherapy, 59(11), 6733-6740.
Alonso, A., Campanario, E., & Martı́nez, J. L. (1999). Emergence of multidrug-resistant mutants is increased under antibiotic selective pressure in Pseudomonas aeruginosa. Microbiology, 145(10), 2857-2862.
Causes of antibiotic resistance. Union for International Cancer Control (UICC). Retrieved April 11, 2024, from https://www.uicc.org/resources/causes-antibiotic-resistance
Singh, A. K., Kaur, R., Verma, S., & Singh, S. (2022). Antimicrobials and antibiotic resistance genes in water bodies: pollution, risk, and control. Frontiers in Environmental Science, 10, 830861.
Michael, C. A., Dominey-Howes, D., & Labbate, M. (2014). The antimicrobial resistance crisis: causes, consequences, and management. Frontiers in public health, 2, 110657.
Tang, K. W. K., Millar, B. C., & Moore, J. E. (2023). Antimicrobial resistance (AMR). British Journal of Biomedical Science, 80, 11387.
Suetens, C., Latour, K., Kärki, T., Ricchizzi, E., Kinross, P., Moro, M. L., ... & Healthcare-Associated Infections Prevalence Study Group. (2018). Prevalence of healthcare-associated infections, estimated incidence and composite antimicrobial resistance index in acute care hospitals and long-term care facilities: results from two European point prevalence surveys, 2016 to 2017. Eurosurveillance, 23(46), 1800516.
Jiang, T., & Chen, X. S. (2020). Outcome impacts due to pathogen-specific antimicrobial resistance: A narrative review of published literature. International Journal of Environmental Research and Public Health, 17(4), 1395.
Kashyap, R. S., Nayak, A. R., Husain, A. A., Gaherwar, H. M., Purohit, H. J., Taori, G. M., & Daginawala, H. F. (2013). Tuberculosis in India: the continuing challenge. Current Science, 597-606.
WHO global lists of high burden countries for tuberculosis (TB), TB/HIV and multidrug/rifampicin-resistant TB (MDR/RR-TB), 2021–2025. World Health Organisation. Retrieved April 12, 2024, from https://cdn.who.int/media/docs/default-source/hq-tuberculosis/who_globalhbcliststb_2021-2025_backgrounddocument.pdf?sfvrsn=f6b854c2_9
Hillock, N. T., Merlin, T. L., Turnidge, J., & Karnon, J. (2022). Modelling the future clinical and economic burden of antimicrobial resistance: the feasibility and value of models to inform policy. Applied Health Economics and Health Policy, 20(4), 479-486.
Organisation for Economic Co-operation and Development. (2023). Embracing a One Health Framework to Fight Antimicrobial Resistance. OECD Publishing.
World Bank. (2017). Drug-resistant infections: a threat to our economic future. World Bank.
Bassetti, M., & Giacobbe, D. R. (2020). A look at the clinical, economic, and societal impact of antimicrobial resistance in 2020. Expert opinion on pharmacotherapy, 21(17), 2067-2071.
Innes, G. K., Randad, P. R., Korinek, A., Davis, M. F., Price, L. B., So, A. D., & Heaney, C. D. (2020). External societal costs of antimicrobial resistance in humans attributable to antimicrobial use in livestock. Annual review of public health, 41, 141-157.
Deogaonkar, M. (2004). Socio-economic inequality and its effect on healthcare delivery in India: inequality and healthcare. Electronic Journal of Sociology, 11(2), 25-35.
Arcaya, M. C., Arcaya, A. L., & Subramanian, S. V. (2015). Inequalities in health: definitions, concepts, and theories. Global health action, 8(1), 27106.
Skodvin, B., Wathne, J. S., Lindemann, P. C., Harthug, S., Nilsen, R. M., Charani, E., ... & Smith, I. (2019). Use of microbiology tests in the era of increasing AMR rates–a multicentre hospital cohort study. Antimicrobial Resistance & Infection Control, 8, 1-8.
Ronat, J. B., Natale, A., Kesteman, T., Andremont, A., Elamin, W., Hardy, L., ... & Kouassi, F. (2021). AMR in low-resource settings: Médecins Sans Frontières bridges surveillance gaps by developing a turnkey solution, the Mini-Lab. Clinical Microbiology and Infection, 27(10), 1414-1421.
Ueda, T., Takesue, Y., Nakajima, K., Ichiki, K., Ishikawa, K., Yamada, K., ... & Kimura, T. (2023). Correlation between antimicrobial resistance and the hospital-wide diverse use of broad-spectrum antibiotics by the antimicrobial stewardship program in Japan. Pharmaceutics, 15(2), 518.
Colson, P., & Raoult, D. (2016). Fighting viruses with antibiotics: an overlooked path. International journal of antimicrobial agents, 48(4), 349.
Kasimanickam, V., Kasimanickam, M., & Kasimanickam, R. (2021). Antibiotics use in food animal production: escalation of antimicrobial resistance: where are we now in combating AMR?. Medical Sciences, 9(1), 14.
Haynes, E., Ramwell, C., Griffiths, T., Walker, D., & Smith, J. (2020). Review of antibiotic use in crops, associated risk of antimicrobial resistance and research gaps. Report to Department for Environment, Food and Rural Affairs (Defra) & The Food Standards Agency (FSA), 1-83.
Mshana, S. E., Sindato, C., Matee, M. I., & Mboera, L. E. (2021). Antimicrobial use and resistance in agriculture and food production systems in Africa: a systematic review. Antibiotics, 10(8), 976.
EFSA Panel on Biological Hazards (BIOHAZ), Koutsoumanis, K., Allende, A., Álvarez‐Ordóñez, A., Bolton, D., Bover‐Cid, S., ... & Peixe, L. (2021). Role played by the environment in the emergence and spread of antimicrobial resistance (AMR) through the food chain. EFSA Journal, 19(6), e06651.
Sanderson, H., Brown, R. S., Hania, P., McAllister, T. A., Majury, A., & Liss, S. N. (2019). Antimicrobial-resistant genes and organisms as environmental contaminants of emerging concern: addressing global public health risks. In Management of emerging public health issues and risks (pp. 147-187). Academic Press.
Inoue, H. (2019). Strategic approach for combating antimicrobial resistance (AMR). Global Health & Medicine, 1(2), 61-64.
Combating Antimicrobial Resistance. United States Agency for International Development (USAID). Retrieved April 12, 2024, from https://www.usaid.gov/global-health/health-systems-innovation/health-systems/combating-antimicrobial-resistance#:~:text=Strengthening%20supply%20chains%20to%20ensure,essential%20medicines%20lists%20and%20formularies.
Global Action Plan. World Health Organisation. Retrieved April 12, 2024, from https://www.who.int/initiatives/sdg3-global-action-plan
The Global Antibiotic Research & Development Partnership. GARDP. Retrieved April 12, 2024, from https://gardp.org/
Antimicrobial resistance: Here’s what can be done to address environmental AMR in India. Down To Earth. Retrieved April 12, 2024, from https://www.downtoearth.org.in/blog/health/antimicrobial-resistance-here-s-what-can-be-done-to-address-environmental-amr-in-india-86307
Fazaludeen Koya, S., Ganesh, S., Selvaraj, S., Wirtz, V. J., Galea, S., & Rockers, P. C. (2022). Antibiotic consumption in India: geographical variations and temporal changes between 2011 and 2019. JAC-Antimicrobial Resistance, 4(5), dlac112.
Ranjalkar, J., & Chandy, S. J. (2019). India's National Action Plan for antimicrobial resistance–An overview of the context, status, and way ahead. Journal of family medicine and primary care, 8(6), 1828-1834.
da Silva, A. A., de Almeida Dias, D. A., Marques, A. F., di Biase, C. B., Murni, I. K., Dramowski, A., ... & Zingg, W. (2018). Role of antimicrobial stewardship programmes in children: a systematic review. Journal of Hospital Infection, 99(2), 117-123.
Pierce, J., Apisarnthanarak, A., Schellack, N., Cornistein, W., Al Maani, A., Adnan, S., & Stevens, M. P. (2020). Global Antimicrobial Stewardship with a Focus on Low-and Middle-Income Countries: A position statement for the international society for infectious diseases. International Journal of Infectious Diseases, 96, 621-629.
Core elements of antibiotic stewardship. Global Alliance for Infections in Surgery. Retrieved April 12, 2024, from https://infectionsinsurgery.org/core-elements-of-antibiotic-stewardship/
Welch, H. K., Nagel, J. L., Patel, T. S., Gandhi, T. N., Chen, B., De Leon, J., ... & Eschenauer, G. A. (2016). Effect of an antimicrobial stewardship intervention on outcomes for patients with Clostridium difficile infection. American journal of infection control, 44(12), 1539-1543.
Guah, M. W., & Currie, W. L. (2004, January). Logicality of ASP in healthcare: The NHS case study. In 37th Annual Hawaii International Conference on System Sciences, 2004. Proceedings of the (pp. 10-pp). IEEE.
Johannsson, B., Beekmann, S. E., Srinivasan, A., Hersh, A. L., Laxminarayan, R., Polgreen, P. M., & Infectious Diseases Society of America Emerging Infections Network. (2011). Improving antimicrobial stewardship the evolution of programmatic strategies and barriers. Infection Control & Hospital Epidemiology, 32(4), 367-374.
Ayukekbong, J. A., Ntemgwa, M., & Atabe, A. N. (2017). The threat of antimicrobial resistance in developing countries: causes and control strategies. Antimicrobial Resistance & Infection Control, 6, 1-8.
Kumar, M., Sarma, D. K., Shubham, S., Kumawat, M., Verma, V., Nina, P. B., ... & Tiwari, R. R. (2021). Futuristic non-antibiotic therapies to combat antibiotic resistance: A review. Frontiers in microbiology, 12, 609459.
Murugaiyan, J., Kumar, P. A., Rao, G. S., Iskandar, K., Hawser, S., Hays, J. P., ... & van Dongen, M. B. (2022). Progress in alternative strategies to combat antimicrobial resistance: Focus on antibiotics. Antibiotics, 11(2), 200.
Adesanya, O., Oduselu, T., Akin-Ajani, O., Adewumi, O. M., & Ademowo, O. G. (2020). An exegesis of bacteriophage therapy: An emerging player in the fight against anti-microbial resistance. AIMS microbiology, 6(3), 204.
Parsons, C., Brown, P., & Kathariou, S. (2021). Use of bacteriophage amended with CRISPR-Cas systems to combat antimicrobial resistance in the bacterial foodborne pathogen Listeria monocytogenes. Antibiotics, 10(3), 308.
Kober, A. H., Saha, S., Islam, M. A., Rajoka, M. S. R., Fukuyama, K., Aso, H., ... & Kitazawa, H. (2022). Immunomodulatory effects of probiotics: a novel preventive approach for the control of bovine mastitis. Microorganisms, 10(11), 2255.
Max, B. L., Angolile, C. M., Raymond, V. G., & Mashauri, H. L. (2023). The dawn of repurposing vitamins as potential novel antimicrobial agents: A call for global emergency response amidst AMR crisis. Health Science Reports, 6(5), e1276.
Jorge, P., Magalhães, A. P., Grainha, T., Alves, D., Sousa, A. M., Lopes, S. P., & Pereira, M. O. (2019). Antimicrobial resistance in three ways: healthcare crisis, major concepts and the relevance of biofilms. FEMS microbiology ecology, 95(8), fiz115.
Sivam, V., Rangasamy, A., & Dara, P. K. (2023). Nanoparticle Approach to Control AMR. In Handbook on Antimicrobial Resistance: Current Status, Trends in Detection and Mitigation Measures (pp. 925-946). Singapore: Springer Nature Singapore.
Coates, A. R., Hu, Y., Holt, J., & Yeh, P. (2020). Antibiotic combination therapy against resistant bacterial infections: synergy, rejuvenation and resistance reduction. Expert review of Anti-infective therapy, 18(1), 5-15.
Osman, A. H., Kotey, F. C., Odoom, A., Darkwah, S., Yeboah, R. K., Dayie, N. T., & Donkor, E. S. (2023). The potential of bacteriophage-antibiotic combination therapy in treating infections with multidrug-resistant bacteria. Antibiotics, 12(8), 1329.
Anahtar, M. N., Yang, J. H., & Kanjilal, S. (2021). Applications of machine learning to the problem of antimicrobial resistance: an emerging model for translational research. Journal of Clinical Microbiology, 59(7), 10-1128.
One Health Basics. Centre for Disease Control and Prevention (CDC). Retrieved April 14, 2024, from https://www.cdc.gov/onehealth/basics/index.html#:~:text=One%20Health%20is%20a%20collaborative,plants%2C%20and%20their%20shared%20environment.
White, A., & Hughes, J. M. (2019). Critical importance of a one health approach to antimicrobial resistance. EcoHealth, 16, 404-409.
Antimicrobial Resistance: A Global Threat. United Nations Environment Program (UNEP). Retrieved April 14, 2024, from https://www.unep.org/topics/chemicals-and-pollution-action/pollution-and-health/antimicrobial-resistance-global-threat
Guardabassi, L., Apley, M., Olsen, J. E., Toutain, P. L., & Weese, S. (2018). Optimization of antimicrobial treatment to minimize resistance selection. Antimicrobial Resistance in Bacteria from Livestock and Companion Animals, 637-673.
Sustainable Development Goals. Gavi, The Vaccination Alliance. Retrieved April 14, 2024, from https://www.gavi.org/our-alliance/global-health-development/sustainable-development-goals?gad_source=1&gclid=CjwKCAjw8diwBhAbEiwA7i_sJVz4OjmmtaGt_WJJpZAIkVDw9O2cJim0mrO3Ov0IUjq0sHwMxfaaBBoCaqcQAvD_BwE
TURNING PLANS INTO ACTION FOR ANTIMICROBIAL RESISTANCE (AMR). World Health Organisation. Retrieved April 14, 2024, from https://iris.who.int/bitstream/handle/10665/311386/WHO-WSI-AMR-2019.2-eng.pdf
Copyright (c) 2024 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


