Pulmonary and extrapulmonary tuberculosis, an inflammatory disease misdiagnosed as cancer
Tuberculosis misdiagnosed as cancer
Abstract
Introduction: tuberculosis is a serious infection associated with high mortally rate if not treated. The clinical and imaging presentation are usually nonspecific and can mimic malignancy; therefore, extrapulmonary TB should be considered in the differential diagnosis of any suspicious extrapulmonary masses, particularly in immunocompromised patients.
Objective: the aim of this study is to analyzed 160 case of pulmonary and extra-pulmonary tuberculosis and correlate the pathological features with the clinical data and to find the most common differentiation diagnosis of both pulmonary and extrapulmonary tuberculosis
Methodology: a retrospective analysis of 160 case of pulmonary and extra-pulmonary tuberculosis was performed. The age, the gender, the site, and the symptoms of the lesion were collected, extrapulmonary sites were detected including rare and unusual sites and the differential diagnosis of these lesion was highlighted. The data were plotted in graphs and were analyzed
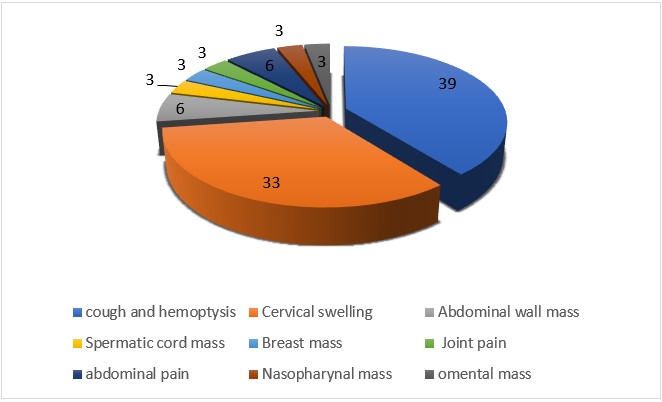
Result: in our study 63.6% were male and 36.4 were females. Majority of the patients were in the age group of 21-30 years followed by 31- 40-year, cough and hemoptysis were the most common symptoms followed by cervical swelling with 39% and 33% respectively. The most common sites were lung with (39%) and cervical swelling with (33%). The main differential diagnosis for many pulmonary and all extra-pulmonary tuberculosis was malignancy
Conclusion: tuberculosis is a serious young person disease that can affect almost every organ and tissue of the body and should be considered in the differential diagnosis of suspicious masses, as tuberculosis often misdiagnosed as cancer
keywords: Mycobacterium tuberculosis, cancer, malignancy, extrapulmonary.
Downloads
References
2. Global tuberculosis report 2020. Geneva: World Health Organization; 2020. Licence: CC BY-NC-SA 3.0 IGO
3. Yang Z, Kong Y, Wilson F, et al. Identification of risk factors for extrapulmonary tuberculosis. Clin Infect Dis. 2004;38: 199–205.
4. Sharma SK, Mohan A. Extra-pulmonary tuberculosis. Indian J Med Res 2004; 120: 316-353.
5. Heye T, Stoijkovic M, Kauczor H, Junghanss T, Hosch W. Extrapulmonary tuberculosis: radiological imaging of an almost forgotten transformation artist. RoFo 2011; 183(11):1019–1029
6. Rodriguez-Takeuchi SY, Renjifo ME, Medina FJ. Extrapulmonary tuberculosis: pathophysiology and imaging findings. Radiographics. 2019; 39(7):2023–2037
7. Sharma SK, Mohan A, Kohli M. Extrapulmonary tuberculosis. Expert Rev Respir Med. 2021;15(7):931–948
8. Bernaerts A, Vanhoenacker F, Parizel P et al. Tuberculosis of the central nervous system: overview of neuroradiological findings. Eur Radiol. 2003;13(8):1876–1890
9. Gambhir S, Ravina M, Rangan K, Dixit M, Barai S, Bomanji J. Imaging in extrapulmonary tuberculosis. Int J Infect Dis. 2017;56:237–247
10. Natarajan A, Beena P, Devnikar AV, Mali S. A systemic review on tuberculosis. Indian J Tuberc. 2020;67:295–311
11. Sardana V, Shringi P. Intramedullary tuberculoma of the spinal cord, clinical features & imaging: possibility of early diagnosis with imaging? Indian J Tuberc. 2019;67(3):346–348
12. Baykan AH, Sayiner HS, Inan I, Aydin E, Erturk SM. Primary breast tuberculosis: imaging findings of a rare disease. Insights Imaging. 2021;12(1):1–11
13. Tewari M, Shukla H. Breast tuberculosis: diagnosis, clinical features & management. Indian J Med Res. 2005;122(2):103
14. Ladumor H, Al-Mohannadi S, Ameerudeen FS, Ladumor S, Fadl S. TB or not TB: a comprehensive review of imaging manifestations of abdominal tuberculosis and its mimics. Clin Imaging. 2021;76:130–143
15. Gibson MS, Puckett ML, Shelly ME. Renal tuberculosis. Radiographics. 2004;24(1):251–256
16. Karaosmanoglu AD, Onur MR, Sahani DV, Tabari A, Karcaaltincaba M. Hepatobiliary tuberculosis: imaging findings. AJR Am J Roentgenol. 2016;207(4):694–704
17. Leonard MK Jr, Blumberg HM (2017) Musculoskeletal tuberculosis. Microbiol. 2017;(9):5(2):5–2
18. Naeem M, Zulfiqar M, Siddiqui MA et al. Imaging manifestations of genitourinary tuberculosis. Radiographics. 2021;41:1123–1143
19. Cowley A, Dobson L, Kurian J, Saunderson C. Acute myocarditis secondary to cardiac tuberculosis: a case report. Echo Res Pract. 2017;4(3):K25
20. Ortiz-Flores A, Gioia F, Montánez-Fernández L et al. Incidental finding of a primary thyroid tuberculosis. Oxford Med Case Rep. 2017;(6):omx022
21. Al-Mulhim A, Zakaria H, Abdel hadi M, Al-Mulhim F, AlTamimi D, Wosornu L. Thyroid tuberculosis mimicking carcinoma: report of two cases. Surg Today. 2002;32:1064 –1067
22. Wu C, Wang S, Kuo T. Pancreatic tuberculosis mimicking pancreatic head carcinoma: a case report and review of the literature. Infection. 1994;22:287–289
23. Orgdorff MW, Nagelkerke NJ, Dye C, Nunn P. Gender and tuberculosis: a comparison of prevalence surveys with notification data to explore sex differences in case detection. Int J Tuberc Lung Dis. 2000;4:123–32
24. Watkins RE, Plant AJ. Does smoking explain sex differences in the global tuberculosis epidemic? Epidemiology and Infection. 2006;134(2):333-339.
25. de Waroux OlP, Cohuet S, Ndazima D, et al. Characteristics of human encounters and social mixing patterns relevant to infectious diseases spread by close contact: A survey in southwest Uganda. bioRxiv; 2017. DOI: 10.1101/121665.
26. Dong, Z., Wang, QQ., Yu, SC. et al. Age–period–cohort analysis of pulmonary tuberculosis reported incidence, China, 2006–2020. Infect Dis Poverty. 2022;11, 85
27. Teo, A., Rahevar, K., Morishita, F. et al. Tuberculosis in older adults: case studies from four countries with rapidly ageing populations in the western pacific region. BMC Public Health 2023;23, 370.
28. Ismail, Yasser. Pulmonary tuberculosis--a review of clinical features and diagnosis in 232 cases. The Medical journal of Malaysia. 2004;59:56-64
29. Piura B, Rabinovich A, Leron E, Yanai-Inbar I, Mazor M. Peritoneal tuberculosis mimicking ovarian carcinoma with ascites and elevated serum CA-125: case report and review of the literature. Eur J Gynaecol Oncol. 2002;23:120–122.
30. Fukasawa H, Suzuki H, Kato A, et al. Tuberculous arthritis mimicking neoplasm in a hemodialysis patient. Am J Med Sci. 2001;322:373–375.
31. Rezeig M, Fashir B, Al-Suhaibani H, Al-Fadda M, Amin T, Eisa H. Pancreatic tuberculosis mimicking pancreatic carcinoma: four case reports and review of the literature. Dig Dis Sci. 1998;43:329–331.
32. Rolston K, Rodriguez S, Dholakia N, Whimbey E, Raad I. Pulmonary infections mimicking cancer: a retrospective, three-year review. Support Care Cancer. 1997;5:90 –93.
33. Jørstad MD, Aẞmus J, Marijani M, Sviland L, Mustafa T. Diagnostic delay in extrapulmonary tuberculosis and impact on patient morbidity: A study from Zanzibar. PLoS One. 2018 Sep 6;13(9)
34. Khan, A.H., Sulaiman, S.A.S., Laghari, M. et al. Treatment outcomes and risk factors of extra-pulmonary tuberculosis in patients with co-morbidities. BMC Infect Dis. 2019;19, 691.
35. Chisale MRO, Sinyiza F, Kaseka P, Wu JST, Chimbatata C, Mbakaya BC, Kamudumuli PS, Kayira AB. Cancer obscures extrapulmonary tuberculosis (EPTB) at a tertiary hospital in Northern Malawi. Epidemiol Infect. 2020;(9):20;149:e3.
Copyright (c) 2024 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


