Expert opinion on the clinical approach of using sodium glucose cotransporter-2 inhibitors for managing diabetic patients with cardiovascular and renal complications in Indian settings
Expert view on sodium glucose cotransporter-2 inhibitors
Abstract
Objective: To evaluate the prescription practice of sodium-glucose co-transporter-2 (SGLT2) inhibitors with a special focus on dapagliflozin to treat cardiac and renal disorders in obese Indian diabetic patients.
Methods: A cross-sectional, questionnaire based study was conducted to collect the perspectives among physicians with expertise in treating diabetic obese patients with cardiac and renal disorders in endocrinology across India between June 2022 and December 2022. Descriptive statistics were used to summarize the characteristics of the study by employing frequencies and percentages.
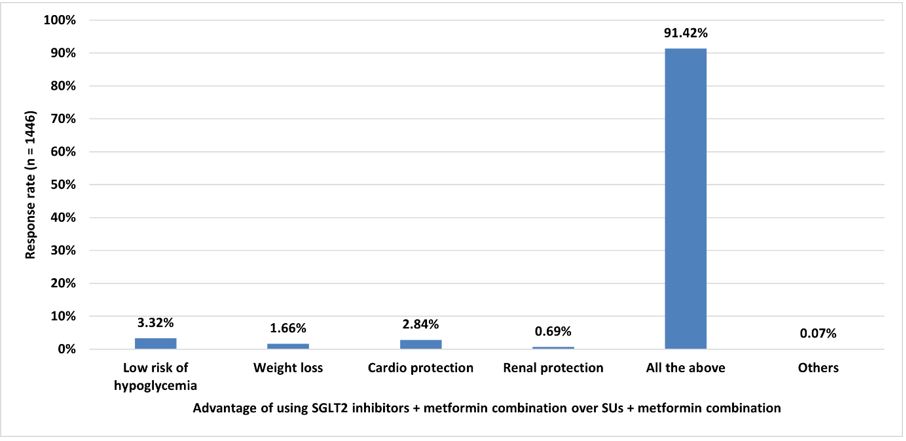
Results: Among the 1,446 survey participants, 80% of them indicated that young diabetic patients with obesity, and obese patients with cardio-renal complications may require SGLT2 inhibitors. Furthermore, patients aged between 41-50 and 51-60 years also required SGLT2 inhibitors for diabetes management according to 57% and 27% of the respondents. The majority of the respondents (91.29% and 90.53%) recommended dapagliflozin as the best SGLT2 inhibitor for treating patients with chronic kidney disease and heart failure. Additionally, about 59% and 66% of the experts indicated that patients would experience an average weight loss of 2-3 kilograms and an average blood pressure reduction of 3-6 mm Hg after 12 weeks of treatment with dapagliflozin, respectively.
Conclusion: Experts recommend the use of SGLT2 inhibitors for the treatment of young diabetic patients with obesity and obese subjects with cardiorenal complications. Dapagliflozin monotherapy was preferred for patients with chronic kidney disease and heart failure. Furthermore, experts highly recommend the combinations of dapagliflozin + metformin and DPP4 inhibitors + metformin + dapagliflozin for effective diabetes management
Downloads
References
2. Ahmad FS, Ning H, Rich JD, et al. Hypertension, Obesity, Diabetes, and Heart Failure–Free Survival. JACC: Heart Failure, 2016;4(12):911–919. doi: 10.1016/j.jchf.2016.08.001.
3. Tsao CW, Aday AW, Almarzooq ZI, et al. Heart Disease and Stroke Statistics-2023 Update: A Report From the American Heart Association. Circulation, 2023;147(8):e93-e621. doi: 10.1161/CIR.0000000000001123.
4. Davies MJ, D'Alessio DA, Fradkin J, et al. Management of Hyperglycemia in Type 2 Diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care, 2018; 41(12):2669-2701. doi: 10.2337/dci18-0033.
5. Hills AP, Arena R, Khunti K, et al. Epidemiology and determinants of type 2 diabetes in South Asia. Lancet Diabetes Endocrinol. 2018;6(12):966-78. doi: 10.1016/S2213-8587(18)30204-3.
6. Shah A, Kanaya AM. Diabetes and associated complications in the South Asian population. Curr Cardiol Rep. 2014;16(5):476. doi: 10.1007/s11886-014-0476-5.
7. Kalra S, Sahay RK, Schnell O, et al. Alpha-glucosidase inhibitor, acarbose, improves glycemic control and reduces body weight in type 2 diabetes: Findings on indian patients from the pooled data analysis. Indian J Endocrinol Metab. 2013;17(Suppl 1):S307-9. doi: 10.4103/2230-8210.119634.
8. Chadha M, Das AK, Deb P, et al. Expert Opinion: Optimum Clinical Approach to Combination-Use of SGLT2i + DPP4i in the Indian Diabetes Setting. Diabetes Ther. 2022;13(5):1097–1114. doi: 10.1007/s13300-022-01219-x.
9. Zargar AH, Trailokya AA, Ghag S, et al. Current Role of Dapagliflozin in Clinical Practice. The Journal of the Association of Physicians of India, 2021;69(9):11-2.
10. Highlights of prescribing information for FARXIGA. FARXIGA® (dapagliflozin) tablets, for oral use Initial U.S. Approval: 2014. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/202293s020lbl.pdf
11. Zelniker TA, Braunwald E. Mechanisms of Cardiorenal Effects of Sodium-Glucose Cotransporter 2 Inhibitors: JACC State-of-the-Art Review. Journal of the American College of Cardiology, 2020;75(4):422–34. doi: 10.1016/j.jacc.2019.11.031.
12. Rajasekeran H, Cherney DZ, Lovshin JA. Do the effects of sodium–glucose cotransporter-2 inhibitors in patients with diabetes give insight into potential use in non-diabetic kidney disease? Current Opinion in Nephrology and Hypertension, 2017;26(5):358. doi: 10.1097/MNH.0000000000000343.
13. Nincevic V, Omanovic Kolaric T, Roguljic H, et al. Renal Benefits of SGLT 2 Inhibitors and GLP-1 Receptor Agonists: Evidence Supporting a Paradigm Shift in the Medical Management of Type 2 Diabetes. International Journal of Molecular Sciences, 2019;20(23):5831. doi: 10.3390/ijms20235831.
14. Chilton RJ. Effects of sodium-glucose cotransporter-2 inhibitors on the cardiovascular and renal complications of type 2 diabetes. Diabetes, Obesity and Metabolism, 2020;22(1):16–29. doi: 10.1111/dom.13854.
15. Ni L, Yuan C, Chen G, Zhang C, Wu X. SGLT2i: beyond the glucose-lowering effect. Cardiovascular Diabetology, 2020;19(1):98. doi: 10.1186/s12933-020-01071-y.
16. Henry RR, Thakkar P, Tong C, Polidori D, Alba M. Efficacy and Safety of Canagliflozin, a Sodium–Glucose Cotransporter 2 Inhibitor, as Add-on to Insulin in Patients With Type 1 Diabetes. Diabetes Care, 2015;38(12):2258–65. doi: 10.2337/dc15-1730.
17. Dandona P, Mathieu C, Phillip M, et al. Efficacy and safety of dapagliflozin in patients with inadequately controlled type 1 diabetes (DEPICT-1): 24-week results from a multicentre, double-blind, phase 3, randomised controlled trial. The Lancet Diabetes & Endocrinology, 2017;5(11):864–76. doi: 10.1016/S2213-8587(17)30308-X.
18. Henry RR, Murray AV, Marmolejo MH, et al. Dapagliflozin, metformin XR, or both: initial pharmacotherapy for type 2 diabetes, a randomised controlled trial. International Journal of Clinical Practice, 2012;66(5):446–56. doi: 10.1111/j.1742-1241.2012.02911.x.
19. Bailey CJ, Gross JL, Pieters A, Bastien A, List JF. Effect of dapagliflozin in patients with type 2 diabetes who have inadequate glycaemic control with metformin: a randomised, double-blind, placebo-controlled trial. The Lancet, 2010;375(9733):2223–33. doi: 10.1016/S0140-6736(10)60407-2.
20. Lee S, Lee H, Kim Y, Kim E. Effect of DPP-IV Inhibitors on Glycemic Variability in Patients with T2DM: A Systematic Review and Meta-Analysis. Sci Rep. 2019;9(1):13296. doi: 10.1038/s41598-019-49803-9.
21. Lee H, Park SE, Kim EY. Glycemic Variability Impacted by SGLT2 Inhibitors and GLP 1 Agonists in Patients with Diabetes Mellitus: A Systematic Review and Meta-Analysis. J Clin Med. 2021;10(18):4078. doi: 10.3390/jcm10184078.
22. Anoop S, Misra A, Bhatt SP, et al. High circulating plasma dipeptidyl peptidase- 4 levels in non-obese Asian Indians with type 2 diabetes correlate with fasting insulin and LDL-C levels, triceps skinfolds, total intra-abdominal adipose tissue volume and presence of diabetes: a case-control study. BMJ Open Diabetes Res Care. 2017;5(1):e000393. doi: 10.1136/bmjdrc-2017-000393.
23. Gan S, Dawed AY, Donnelly LA, et al. Efficacy of Modern Diabetes Treatments DPP-4i, SGLT-2i, and GLP-1RA in White and Asian Patients With Diabetes: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Diabetes Care, 2020;43(8):1948–57. doi: 10.2337/dc19-2419.
24. Kaku K, Lee J, Mattheus M, et al. Empagliflozin and Cardiovascular Outcomes in Asian Patients With Type 2 Diabetes and Established Cardiovascular Disease ― Results From EMPA-REG OUTCOME® ―. Circulation Journal, 2017;81(2):227–234. doi: 10.1253/circj.CJ-16-1148.
25. Kaku K, Haneda M, Tanaka Y, et al. Linagliptin as add-on to empagliflozin in a fixed-dose combination in Japanese patients with type 2 diabetes: Glycaemic efficacy and safety profile in a two-part, randomized, placebo-controlled trial. Diabetes, Obesity and Metabolism, 2019;21(1):136–145. doi: 10.1111/dom.13496.
Copyright (c) 2024 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


