The Effect Of Umbilical Cord Milking In Reducing ROP Of Preterm Babies.
Abstract
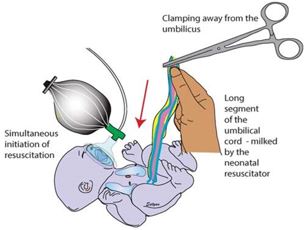
Background: Recent advances in neonatal care in the last decade have improved the survival rates for premature infants. Consequently, the incidence of ROP has increased in parallel. ROP is under constant epidemiological study around the world. Prematurity, low birth weight, respiratory distress syndrome, mechanical ventilation, prolonged oxygen treatment and blood transfusion increase the risk of ROP. Umbilical cord milking reduces the incidence of ROP in preterm infants by reducing the need for blood transfusions in preterm infants. Objective: To observe effect of ROP with umbilical cord milking. Methodology: This prospective observational study was carried out on neonates, in the Department of Neonatology, BSMMU after approval from IRB. Neonates admitted into neonatal intensive care unit of BSMMU satisfying the inclusion and exclusion criteria was enrolled for the study. A written informed consent was taken from parents and assurance about confidentiality was given. Neonates born before 37 weeks of gestation was assigned to either umbilical cord milking or non-milking group at a 1: 1 ratio according to a computer generated randomized sequence. After delivery of a baby umbilical cord milking was performed by holding the infant at the level of the placenta. First eye evaluation for ROP was done at 20 days of age for gestational age less than 30weeks & weight below 1200gm & at 30 days of age for gestational age more than 30 weeks & above weight 1200gm. Follow-up was continued until retinal vascularization was completed. The follow-up schedules were organized depending on the retinal findings. The retinal finding was evaluated according to the International Classification of Retinopathy of Prematurity. The patients were grouped as no ROP, mild ROP (stages I-II ROP without plus disease, showed regression), and severe ROP (zone 1 or zone 2, stage III, aggressive ROP without stages, stage II with plus disease who required treatment). Data were recorded in a preformed questionnaire and data were analyzed by statistical package for social sciences (SPSS) version 20. Results: 114 newborns were enrolled in this study. Then among 114 preterm neonates 57 were randomized to umbilical cord milking group and 57 were randomized to no milking group. Baseline characteristics were almost similar between the two groups. There were significant increase is hematocrit level 57.3 ±3.5 V 47.4 ± 4.5 (P value less than 0.001), reduction in need of blood transfusion 3.5% V 42.1% (P value less than 0.001) & reduction in ROP 3.5% V 19.3% (P 0.007). Conclusion: This study concluded that umbilical cord milking after delivery improves hematocrit level, reduces need of blood transfusion & reduces the incidence of ROP in preterm infant.
Downloads
References
1. Lane, S., MacDonald, N. E., Marti, M., & Dumolard, L. (2018). Vaccine hesitancy around the globe: Analysis of three years of WHO/UNICEF Joint Reporting Form data-2015–2017. Vaccine, 36(26), 3861-3867.
2. World Health Organization. (2018). WHO report on surveillance of antibiotic consumption: 2016-2018 early implementations.
3. Gilbert, C. (2008) ‘Retinopathy of prematurity: A global perspective of the epidemics, population of babies at risk and implications for control’, Early Human Development, 84(2), pp. 77–82. doi: 10.1016/j.earlhumdev.2007.11.009.
4. Chirico, G. et al. (1997) ‘Italian multicentre study on retinopathy of prematurity’, European Journal of Pediatrics, 156(12), pp. 939–943. doi: 10.1007/s004310050747.
5. Basile, S. et al. (2019) ‘Milking of the Umbilical Cord in Term and Late Preterm Infants’, BioMed Research International, 2019. doi: 10.1155/2019/9185059.
6. Fogarty, M. et al. (2018) ‘Delayed vs early umbilical cord clamping for preterm infants: a systematic review and meta-analysis’, American Journal of Obstetrics and Gynecology, 218(1), pp. 1–18. doi: 10.1016/j.ajog.2017.10.231.
7. World Health Organization. (2012). Good health adds life to years: Global brief for World Health Day 2012 (No. WHO/DCO/WHD/2012.2). World Health Organization.
8. Katheria, A. C. et al. (2015) ‘Umbilical cord milking versus delayed cord clamping in preterm infants’, Pediatrics, 136(1), pp. 61–69. doi: 10.1542/peds.2015-0368.
9. Kal, A., Silahli, M. and Toprak, E. (2018) ‘ORIGINAL ARTICLE / KLİNİK ÇALIŞMA Relationship Between Umbilical Cord Milking and Development of Retinopathy of Prematurity Umbilikal Kordon Sa ğ lamas ı yla Prematüre Retinopatisi Geli ş imi’, (January).
10. Prematurity*, C. of R. of (2005) ‘The International Classification of Retinopathy of Prematurity Revisited’, Archives of OAlavi, A. et al. (2018) ‘Effect of Umbilical Cord Milking on Neonatal Outcomes among the Preterm Infants Born in Shariati Hospital of Bandar Abbas’, Journal of Research in Medical and Dental Science |, 6(1), pp. 133–139. doi: 10.24896/jrmds.20186121.
11. Committee on Obstetric Practice, A. C. of O. and G. C. O. N. 543. T. of umbilical cord clamping after birth. O. G. 2012 D.-6. doi: 10. 1097/01. A. 0000423817. 47165. 48. P. 23168790. (no date) ‘No Title’.
12. Balasubramanian, S., Rao, N. M., Goenka, A., Roderick, M., & Ramanan, A. V. (2020). Coronavirus disease 2019 (COVID-19) in children-what we know so far and what we do not. Indian pediatrics, 57, 435-442.
13. Gupta, R., & Ramji, S. (2002). Effect of delayed cord clamping on iron stores in infants born to anemic mothers: a randomized controlled trial. Indian pediatrics, 39(2), 130-135.
14. Alavi, A. et al. (2018) ‘Effect of Umbilical Cord Milking on Neonatal Outcomes among the Preterm Infants Born in Shariati Hospital of Bandar Abbas’, Journal of Research in Medical and Dental Science , 6(1), pp. 133–139. doi: 10.24896/jrmds.20186121.
15. Middleton, B., Bloomrosen, M., Dente, M. A., Hashmat, B., Koppel, R., Overhage, J. M. ... & Zhang, J. (2013). Enhancing patient safety and quality of care by improving the usability of electronic health record systems: recommendations from AMIA. Journal of the American Medical Informatics Association, 20(e1), e2-e8.
16. Anderson, L. S., & Heyne, L. A. (2012). Flourishing through leisure: An ecological extension of the leisure and well-being model in therapeutic recreation strengths-based practice. Therapeutic Recreation Journal, 46(2), 129.
17. Oxford Midwives Research Group. (1991). A study of the relationship between the delivery to cord clamping interval and the time of cord separation. Midwifery, 7(4), 167-176.
18. Erickson-Owens, D. A., Mercer, J. S., & Oh, W. (2012). Umbilical cord milking in term infants delivered by cesarean section: a randomized controlled trial. Journal of Perinatology, 32(8), 580-584.
19. Weintraub Z, Carmi N, Elouti H, Rumelt S. The association between stage 3 or higher retinopathy of prematurity and other disorders of prematurity. Can J Ophthalmol. 2011 Oct;46(5):419-24. doi: 10.1016/j.jcjo.2011.07.014. Epub 2011 Aug 4. PMID: 21995985.No’ (no date)
20. Good WV, Hardy RJ, Dobson V, Palmer EA, Phelps DL, Quintos M, Tung B; Early Treatment for Retinopathy of Prematurity Cooperative Group. The incidence and course of retinopathy of prematurity: findings from the early treatment for retinopathy of prematurit’ (no date).
Copyright (c) 2023 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


