New Onset of Diabetes in Adults with Post-Covid Infection in a TertiaryCare Hospital
Abstract
Aim/Scope: This study is aimed to investigate the incidence of diabetes after infection with thecoronavirus (COVID-19). SARS COV2 is a rapidly spreading disease which causes morbidity andmortality. One of the most important complications associated with covid 19 is Diabetes Mellitus.
Materials & Methods: This was a retrospective descriptive study of (50 diabetic and 50 non-diabetic) patients who had a previous history of covid-19 and who are infected during the secondwave (Aug’21-Oct’21) at a tertiary care hospital, Hyderabad, India. Data collected including patientdemographic and baseline characteristics like patient’s age, sex and history of covid infection wereanalyzed using Statistical Package for Social Sciences (SPSS) software version 22.0.
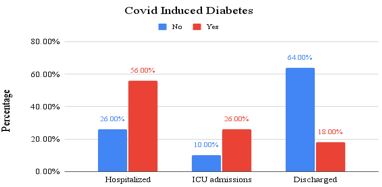
Results: In thestudy among covid infected(n=50) subjects who were tested diabetic after Long Covid, 28(56%)were hospitalized, 13(26%) were found to have ICU admissions and 9(18%) were discharged withmild covid symptoms and the subjects(n=50) who didn’t have any symptoms of diabetes after LongCovid, majority 32(64%) were found to be discharged with mild covid symptoms, 5(10%) werefound to have ICU admissions and 13 (26%)were found to be hospitalized with the critical covidcondition. It was observed that patients hospitalized with critical covid conditions were susceptible toonset of diabetes (p-value: 0.10)
Conclusion: This study showed a high incidence of complicationsin patients infected with COVID-19 with diabetes being the most common one. Patients with poorglycemic control should be routinely monitored and treated appropriately
Downloads
References
[2] Pal R, Bhadada SK, Misra A. Resurgence of COVID-19 and diabetes in India. Diabetes Metab Syndr. 2021 May-Jun; 15(3):1037-1038. Doi: 10.1016/j.dsx.2021.04.024. Epub 2021 May 7. PMID: 34004526; PMCID: PMC8102081.
[3] Pal R, Banerjee M. COVID-19 and the endocrine system: exploring the unexplored. J Endocrinol Invest. 2020 Jul; 43(7):1027-1031. Doi: 10.1007/s40618-020-01276-8. Epub 2020 May 2. PMID: 32361826; PMCID: PMC7195612.
[4]Ayoubkhani D, Khunti K, Nafilyan V, Maddox T, Humberstone B, Diamond I, Banerjee A. Post-covid syndrome in individuals admitted to hospital with covid-19: retrospective cohort study. BMJ. 2021 Mar 31;372:n693. doi: 10.1136/bmj.n693. PMID: 33789877; PMCID: PMC8010267.
[5] Scheen AJ, Marre M, Thivolet C. Prognostic factors in patients with diabetes hospitalized for COVID-19: Findings from the CORONADO study and other recent reports. Diabetes Metab. 2020 Sep;46(4):265-271. doi: 10.1016/j.diabet.2020.05.008. Epub 2020 May 21. PMID: 32447101; PMCID: PMC7241378.
[6] Drucker DJ. Coronavirus Infections and Type 2 Diabetes-Shared Pathways with Therapeutic Implications. Endocr Rev. 2020 Jun 1;41(3):bnaa011. doi: 10.1210/endrev/bnaa011. PMID: 32294179; PMCID: PMC7184382.
[7]Lim, S., Bae, J.H., Kwon, HS. et al. COVID-19 and diabetes mellitus: from pathophysiology to clinical management. Nat Rev Endocrinol 17, 11–30 (2021). https://doi.org/10.1038/s41574-020-00435-4
[8] Liu F, Long X, Zou W, Fang M, Wu W, Li W, et al. (2020) Highly ACE2 expression in pancreas may cause pancreas damage after SARS-CoV-2 infection [Internet] [cited 2020 Apr 1]. Available from: https://medrxiv.org/lookup/doi/10.1101/2020.02.28.20029181.
[9]&[10] Steenblock C, Richter S, Berger I, Barovic M, Schmid J, Schubert U, Jarzebska N, von Mässenhausen A, Linkermann A, Schürmann A, Pablik J, Dienemann T, Evert K, Rodionov RN, Semenova NY, Zinserling VA, Gainetdinov RR, Baretton G, Lindemann D, Solimena M, Ludwig B, Bornstein SR. Viral infiltration of pancreatic islets in patients with COVID-19. Nat Commun. 2021 Jun 10;12(1):3534. doi: 10.1038/s41467-021-23886-3. PMID: 34112801; PMCID: PMC8192507.
[11] Yang JK, Lin SS, Ji XJ, Guo LM. Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes. Acta Diabetol. 2010 Sep;47(3):193-9. doi: 10.1007/s00592-009-0109-4. Epub 2009 Mar 31. PMID: 19333547; PMCID: PMC7088164.
[12] Reiterer, M., Rajan, M., Gómez-Banoy, N., Lau, J. D., Gomez-Escobar, L. G., Gilani, A., ... & Lo, J. C. (2021). Hyperglycemia in acute COVID-19 is characterized by adipose tissue dysfunction and insulin resistance. MedRxiv.
[13] Montefusco L, Ben Nasr M, D'Addio F, Loretelli C, Rossi A, Pastore I, Daniele G, Abdelsalam A, Maestroni A, Dell'Acqua M, Ippolito E, Assi E, Usuelli V, Seelam AJ, Fiorina RM, Chebat E, Morpurgo P, Lunati. Acute and long-term disruption of glycometabolic control after SARS-CoV-2 infection. Nat Metab. 2021 Jun;3(6):774-785. doi: 10.1038/s42255-021-00407-6. Epub 2021 May 25. PMID: 34035524.
[14]Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 Mar 28;395(10229):1054-1062. doi: 10.1016/S0140-6736(20)30566-3. Epub 2020 Mar 11. Erratum in: Lancet. 2020 Mar 28;395(10229):1038. Erratum in: Lancet. 2020 Mar 28;395(10229):1038. PMID: 32171076; PMCID: PMC7270627.
[15] Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020 Apr 7;323(13):1239-1242. doi: 10.1001/jama.2020.2648. PMID: 32091533.
[16] Metwally AA, Mehta P, Johnson BS, Nagarjuna A, Snyder MP. COVID-19-Induced New-Onset Diabetes: Trends and Technologies. Diabetes. 2021 Dec;70(12):2733-2744. doi: 10.2337/dbi21-0029. Epub 2021 Oct 22. PMID: 34686519; PMCID: PMC8660988.
Copyright (c) 2022 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


