Quality Improvement Project in the introduction of Major Trauma and Major Haemorrhage Protocol
Abstract
Introduction: We recognised there was a need for a set criterion for the activation of MHP andMTTA at our Trust. The main aim is to streamline the trauma care that our patients would receivearound the clock. Ours is a large Major Trauma Unit regularly receiving a large volume of traumapatients of varying severity of injury
Objective: The use of a checklist for the initial management of MTTA and MHP to ensure the process is streamlined and led by the trauma team leader. This wouldhelp reduce the cognitive load that is often presented to the team leader. This would also help directjunior team members with limited experience in the initial management of major trauma.
Method/Intervention: An initial survey about MTTA and MHP from senior clinicians was carriedout. Several teaching sessions were undertaken. In addition to this, an algorithm for the initialmanagement in terms of transfer protocol was also introduced.
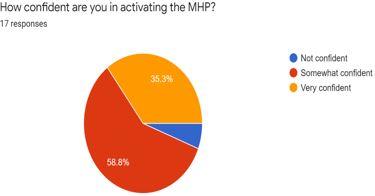
Results: From the clinicians’perspective, 89% of the respondents felt that the use of MHP and MTTA protocol would reduce thecognitive load whilst managing major trauma. There was an improvement in the level of confidenceof clinicians in the initial management of major trauma from 52.9 % to 89%.
Conclusion: Throughthis project, we hope that there is a better understanding of the need to have pre-defined criteria foractivation for MTTA and MTP for several reasons as highlighted in the article. The eventual aim of theproject is to streamline the initial management of the majorly injured patient and undertake thenecessary practical steps.
Downloads
References
doi: 10.11622/smedj.2016031. PMID: 26892937; PMCID: PMC4759378.
2) NWAS - North West Ambulance Service. 2022. MERIT doctor - NWAS - North West Ambulance Service. [online] Available at:
3) Vinjevoll OP, Uleberg O, Cole E. Evaluating the ability of a trauma team activation tool to identify severe injury: a multicentre cohort study. Scand J Trauma Resusc Emerg Med. 2018; 26(1):63
doi: 10.1186/s13049-018-0533-y. PMID: 30097047; PMCID: PMC6086062.
4) Rehn M, Perel P, Blackhall K, Lossius HM. Prognostic models for the early care of trauma patients: a systematic review. Scand J Trauma Resusc Emerg Med. 2011; (19):17
doi: 10.1186/1757-7241-19-17. PMID: 21418599; PMCID: PMC3068084.
5) MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, et al. A National Evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006; 354(4):366–78.
doi: 10.1056/NEJMsa052049. PMID: 16436768
6) Newgard CD, Uribe-Leitz T, Haider AH. Undertriage remains a vexing problem for even the Most highly developed trauma systems: the need for innovations in field triage. JAMA Surg. 2018; 153(4):328.
doi: 10.1001/jamasurg.2017.4499. PMID: 29094149
7) Roberts I, Shakur H, Coats T, Hunt B, Balogun E, Barnetson L,et al. . The CRASH-2 trial: a randomised controlled trial and economic evaluation of the effects of tranexamic acid on death, vascular occlusive events and transfusion requirement in bleeding trauma patients. Health Technol Assess. 2013 Mar;17(10):1-79.
doi: 10.3310/hta17100. PMID: 23477634; PMCID: PMC4780956.
8) Shah B.A., Subramanium A., Sharma S., Agrawal D., Chhabra G., Mukhopadhyay AK.; Thromboelastography - Viscoelastic Haemostatic Assay (VHA) Versus Routine Plasma Based Coagulation Parameters in Trauma Patients to Detect Coagulopathy within 24 Hrs After Injury. Blood 2011; 118 (21): 5248.
Copyright (c) 2022 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


