Risk Factors Affecting Exacerbation of Bronchiectasis Leading to Hospitalisation In Patients Attending A Tertiary Care Setting
Abstract
Introduction: Bronchiectasis is a chronic respiratory disease characterized by structural changes in airways, leading to recurrent episodes of cough with expectoration. Exacerbations are significant events associated with increased morbidity and mortality.
Aim: To evaluate factors associated with exacerbations requiring hospitalization in patients with bronchiectasis
Materials and methods: A prospective observational study was done at a tertiary care teaching hospital from December 2017 to May 2019. Demographic data, comorbidities, investigations including HRCT, sputum culture and spirometry were collected. Patients were grouped into exacerbations requiring hospitalizations and those managed as outpatients and followed up for one year. Factors associated with exacerbations were assessed and compared between the two groups.
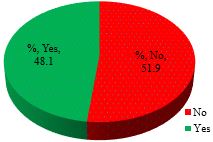
Results: 89 patients were recruited for the study, out of which 12 patients without exacerbation during the study period were excluded. The remaining 77 patients were divided into those who needed hospitalization (37) and those managed as outpatients (40). About 48.1%required hospital admission. Factors associated with exacerbations were advanced age, isolation of organisms from sputum, FEV1 less than 50%, PPI use during the study period, concomitant COPD, vaccination with pneumococcal and influenza vaccines and high severity scores. Use of LTO2, LABA/ICS, chest physiotherapy, mucolytic agents, radiological extent and previous history of exacerbations were not associated with exacerbations leading to hospitalization.
Conclusion: Factors associated with bronchiectasis exacerbations leading to hospitalizations were advanced age, high bronchiectasis severity score, FEV1 less than 50%, PPI use and concomitant COPD. Vaccination for influenza and pneumococcus had a favourable impact in reducing hospitalization.
Downloads
References
Martínez-García MA, Soler-Cataluña JJ, Perpiñá-Tordera M, Román-Sánchez P, Soriano J. Factors associated with lung function decline in adult patients with stable non-cystic fibrosis bronchiectasis. Chest. 2007 Nov;132(5):1565-72. doi: 10.1378/chest.07-0490.
Quint JK, Millett ER, Joshi M, Navaratnam V, Thomas SL, Hurst JR, et al. Changes in the incidence, prevalence and mortality of bronchiectasis in the UK from 2004 to 2013: a population-based cohort study. Eur Respir J. 2016 Jan;47(1):186-93. doi: 10.1183/13993003.01033-2015.
Chalmers JD, Smith MP, McHugh BJ, Doherty C, Govan JR, Hill AT. Short- and long-term antibiotic treatment reduces airway and systemic inflammation in non-cystic fibrosis bronchiectasis. Am J Respir Crit Care Med. 2012 Oct 1;186(7):657-65. doi: 10.1164/rccm.201203-0487OC.
Onen ZP, Gulbay BE, Sen E, Yildiz OA, Saryal S, Acican T, Karabiyikoglu G. Analysis of the factors related to mortality in patients with bronchiectasis. Respir Med. 2007 Jul;101(7):1390-7. doi: 10.1016/j.rmed.2007.02.002.
Dupont M, Gacouin A, Lena H, Lavoué S, Brinchault G, Delaval P, et al. Survival of patients with bronchiectasis after the first ICU stay for respiratory failure. Chest. 2004 May;125(5):1815-20. doi: 10.1378/chest.125.5.1815.
Finklea JD, Khan G, Thomas S, Song J, Myers D, Arroliga AC. Predictors of mortality in hospitalized patients with acute exacerbation of bronchiectasis. Respir Med. 2010 Jun;104(6):816-21. doi: 10.1016/j.rmed.2009.11.021.
Goeminne PC, Nawrot TS, Ruttens D, Seys S, Dupont LJ. Mortality in non-cystic fibrosis bronchiectasis: a prospective cohort analysis. Respir Med. 2014 Feb;108(2):287-96. doi: 10.1016/j.rmed.2013.12.015.
Menéndez R, Méndez R, Polverino E, Rosales-Mayor E, Amara-Elori I, Reyes S, et al. Factors associated with hospitalization in bronchiectasis exacerbations: a one-year follow-up study. Respir Res. 2017 Sep 30;18(1):176. doi: 10.1186/s12931-017-0659-x.
Pasteur MC, Bilton D, Hill AT; British Thoracic Society Bronchiectasis non-CF Guideline Group. British Thoracic Society guideline for non-CF bronchiectasis. Thorax. 2010 Jul;65 Suppl 1:i1-58. doi: 10.1136/thx.2010.136119.
Global strategyfor diagnosis, management and prevention of COPD 2017 UPDATE; e GOLD website www.goldcopd.org.
Pasteur MC, Helliwell SM, Houghton SJ, Webb SC, Foweraker JE, Coulden RA, et al. An investigation into causative factors in patients with bronchiectasis. Am J Respir Crit Care Med. 2000 Oct;162(4 Pt 1):1277-84. doi: 10.1164/ajrccm.162.4.9906120.
Ringshausen FC, de Roux A, Diel R, Hohmann D, Welte T, Rademacher J. Bronchiectasis in Germany: a population-based estimation of disease prevalence. Eur Respir J. 2015 Dec;46(6):1805-7. doi: 10.1183/13993003.00954-2015.
Roberts HR, Wells AU, Milne DG, Rubens MB, Kolbe J, Cole PJ, et al. Airflow obstruction in bronchiectasis: correlation between computed tomography features and pulmonary function tests. Thorax. 2000 Mar;55(3):198-204. doi: 10.1136/thorax.55.3.198.
Davies G, Wells AU, Doffman S, Watanabe S, Wilson R. The effect of Pseudomonas aeruginosa on pulmonary function in patients with bronchiectasis. Eur Respir J. 2006 Nov;28(5):974-9. doi: 10.1183/09031936.06.00074605.
Chalmers JD, Aliberti S, Blasi F. Management of bronchiectasis in adults. Eur Respir J. 2015 May;45(5):1446-62. doi: 10.1183/09031936.00119114.
Finch S, McDonnell MJ, Abo-Leyah H, Aliberti S, Chalmers JD. A Comprehensive Analysis of the Impact of Pseudomonas aeruginosa Colonization on Prognosis in Adult Bronchiectasis. Ann Am Thorac Soc. 2015 Nov;12(11):1602-11. doi: 10.1513/AnnalsATS.201506-333OC.
Jackson MA, Goodrich JK, Maxan ME, Freedberg DE, Abrams JA, et al. Proton pump inhibitors alter the composition of the gut microbiota. Gut. 2016 May;65(5):749-56. doi: 10.1136/gutjnl-2015-310861.
Schuijt TJ, Lankelma JM, Scicluna BP, de Sousa e Melo F, Roelofs JJ, de Boer JD, et al. The gut microbiota plays a protective role in the host defence against pneumococcal pneumonia. Gut. 2016 Apr;65(4):575-83. doi: 10.1136/gutjnl-2015-309728.
Chalmers JD, Goeminne P, Aliberti S, McDonnell MJ, Lonni S, Davidson J, et al. The bronchiectasis severity index. An international derivation and validation study. Am J Respir Crit Care Med. 2014 Mar 1;189(5):576-85. doi: 10.1164/rccm.201309-1575OC.
Alzeer AH, Masood M, Basha SJ, Shaik SA. Survival of bronchiectatic patients with respiratory failure in ICU. BMC Pulm Med. 2007 Dec 10;7:17. doi: 10.1186/1471-2466-7-17.
Martinez-Garcia MA, Athanazio RA, Girón R, Máiz-Carro L, de la Rosa D, Olveira C, et al. Predicting high risk of exacerbations in bronchiectasis: the E-FACED score. Int J Chron Obstruct Pulmon Dis. 2017 Jan 18;12:275-284. doi: 10.2147/COPD.S121943.
Rosales-Mayor E, Polverino E, Raguer L, Alcaraz V, Gabarrus A, Ranzani O, et al. Comparison of two prognostic scores (BSI and FACED) in a Spanish cohort of adult patients with bronchiectasis and improvement of the FACED predictive capacity for exacerbations. PLoS One. 2017 Apr 6;12(4):e0175171. doi: 10.1371/journal.pone.0175171.
McDonnell MJ, Aliberti S, Goeminne PC, Restrepo MI, Finch S, Pesci A, et al. Comorbidities and the risk of mortality in patients with bronchiectasis: an international multicentre cohort study. Lancet Respir Med. 2016 Dec;4(12):969-979. doi: 10.1016/S2213-2600(16)30320-4.
Aliberti S, Mantero M, Mirsaeidi M, Blasi F. The role of vaccination in preventing pneumococcal disease in adults. Clin Microbiol Infect. 2014 May;20 Suppl 5(0 5):52-8. doi: 10.1111/1469-0691.12518.
Peinado VI, Barberá JA, Abate P, Ramírez J, Roca J, Santos S, Rodriguez-Roisin R. Inflammatory reaction in pulmonary muscular arteries of patients with mild chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1999 May;159(5 Pt 1):1605-11. doi: 10.1164/ajrccm.159.5.9807059.
Copyright (c) 2022 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


