A Comparative Evaluation on the effect of Zinc-Probiotic combination versus Zinc alone therapy in children (3month-5year) with acute watery diarrhea attending the outpatient clinic of Sub-District hospital, Uttarakhand
Abstract
Background: Diarrhea is the major cause of morbidity and mortality among children worldwide. Various studies were done on the role of zinc therapy and probiotic therapy in reducing the duration and severity of acute watery diarrhea. This study aimed to compare the effect of Zinc –probiotic combination versus Zinc only therapy in acute watery diarrhea in pediatric patients.
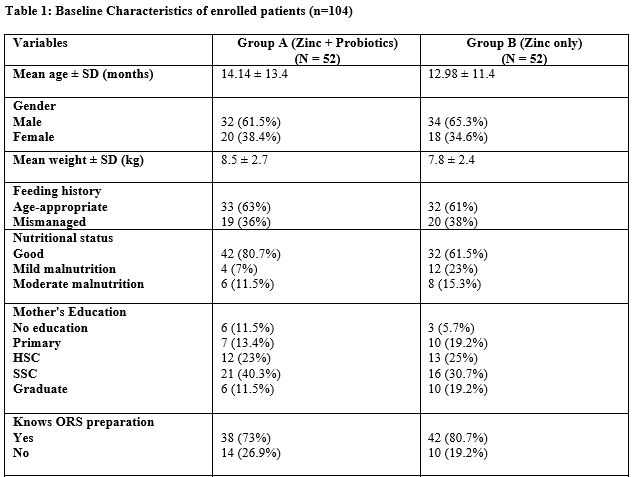
Material and Methods: This was an open, randomized control trial in the pediatric outpatient department of Sub-District Female Hospital, Haldwani (Uttarakhand), from June 2020 till August 2020 for three months. Total 104 children aged six months to 5 years with acute diarrhea who met the inclusion criteria were enrolled and divided into 52 patients each. 1st Group A (n=52) received Zinc-Probiotics combination therapy, and 2ndGroup B (n=52) received Zinc only. Measurement of disease severity was based on the frequency of diarrhea (times/day) and duration of diarrhea (hours) after initial drug consumption. The resolution was assessed in mean remission time (time required to form solid stool from watery stool).
Result: Among the study population in group A, 62% were male, 38% were female, and in group B, 65% were male & 35% were female. Male predominance was observed in both groups. The mean frequency of diarrhea before treatment in Group A was 7.46 ± 4.1 times/day as compared to 6.69 ± 3.6 times/day in Group B. Mean duration of diarrhea in Group A was 53.5 ± 30.5 hours as compared to 57.6 ± 34.3 hours in Group B.
Conclusion: Combination therapy was more effective than Zinc only therapy in early remission and resolution of acute watery diarrhea in children.
Downloads
References
WHO, UNICEF. "End preventable deaths: global action plan for prevention and control of pneumonia and diarrhoea." Geneva: World Health Organization (2013).
Liu L, Oza S, Hogan D, Perin J, Rudan I, Lawn JE, et al. Global, regional, and national causes of child mortality in 2000-13, with projections to inform post-2015 priorities: an updated systematic analysis. Lancet. 2015 Jan 31;385(9966):430-40. doi: 10.1016/S0140-6736(14)61698-6.
Walker CLF, Rudan I, Liu L, Nair H, Theodoratou E, Bhutta ZA, et al. Global burden of childhood pneumonia and diarrhoea. Lancet. 2013 Apr 20;381(9875):1405-1416. doi: 10.1016/S0140-6736(13)60222-6.
Das JK, Salam RA, Bhutta ZA. Global burden of childhood diarrhea and interventions. CurrOpin Infect Dis. 2014 Oct;27(5):451-8. doi: 10.1097/QCO.0000000000000096.
Brown KH. Diarrhea and malnutrition. J Nutr. 2003 Jan;133(1):328S-332S. doi: 10.1093/jn/133.1.328S.
WHO, UNICEF. "WHO-UNICEF Joint statement on the clinical management of acute diarrhea." World Health Assembly. Geneva (2004).
Guandalini S. Probiotics for prevention and treatment of diarrhea. J Clin Gastroenterol. 2011 Nov;45 Suppl:S149-53. doi: 10.1097/MCG.0b013e3182257e98.
Plaza-Diaz J, Ruiz-Ojeda FJ, Gil-Campos M, Gil A. Mechanisms of Action of Probiotics. Adv Nutr. 2019 Jan 1;10(suppl_1):S49-S66. doi: 10.1093/advances/nmy063. Erratum in: Adv Nutr. 2020 Jul 1;11(4):1054.
Allen SJ, Martinez EG, Gregorio GV, Dans LF. Probiotics for treating acute infectious diarrhoea. Cochrane Database Syst Rev. 2010 Nov 10;2010(11):CD003048. doi: 10.1002/14651858.CD003048.pub3. Update in: Cochrane Database Syst Rev. 2020 Dec 8;12:CD003048.
Applegate JA, Fischer Walker CL, Ambikapathi R, Black RE. Systematic review of probiotics for the treatment of community-acquired acute diarrhea in children. BMC Public Health. 2013;13 Suppl 3(Suppl 3):S16. doi: 10.1186/1471-2458-13-S3-S16.
Lewis SJ, Heaton KW. Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol. 1997 Sep;32(9):920-4. doi: 10.3109/00365529709011203.
Azim, M. A., Doza, B., Iqbal, S., Chowdhury, F., & Biswas, S. K. Comparative Evaluation on the Effect of Zinc-Probiotic and Zinc Therapy in Pediatric Acute Gastroenteritis. Chattagram Maa-O-Shishu Hospital Medical College Journal, 19.1 (2020): 74-77.
Nguyen TV, Le Van P, Le Huy C, Weintraub A. Diarrhea caused by rotavirus in children less than 5 years of age in Hanoi, Vietnam. J Clin Microbiol. 2004 Dec;42(12):5745-50. doi: 10.1128/JCM.42.12.5745-5750.2004.
Hatta, M., Supriatmo, S., Ali, M., Sinuhaji, A. B., Hasibuan, B., &Nasution, F. L. Comparison of zinc-probiotic combination therapy to zinc therapy alone in reducing the severity of acute diarrhea. PaediatricaIndonesiana, 51.1. (2011). 1-6.
Sultana, M. M., Islam, M. S., Akhter, S., Hossain, M. B., & Mia, M. S. H. Comparative Study of Zinc and Probiotics versus Zinc Alone Therapy in Children with Acute Watery Diarrhea. TAJ: Journal of Teachers Association, 30.2 (2017): 32-38.
Jarman AF, Long SE, Robertson SE, Nasrin S, Alam NH, McGregor AJ, Levine AC. Sex and Gender Differences in Acute Pediatric Diarrhea: A Secondary Analysis of the DHAKA Study. J Epidemiol Glob Health. 2018 Dec;8(1-2):42-47. doi: 10.2991/j.jegh.2018.08.102.
Bulled N, Singer M, Dillingham R. The syndemics of childhood diarrhoea: a biosocial perspective on efforts to combat global inequities in diarrhoea-related morbidity and mortality. Glob Public Health. 2014;9(7):841-53. doi: 10.1080/17441692.2014.924022.
Desmennu AT, Oluwasanu MM, John-Akinola YO, Oladunni O, Adebowale AS. Maternal Education and Diarrhea among Children aged 0-24 Months in Nigeria. Afr J Reprod Health. 2017 Sep;21(3):27-36. doi: 10.29063/ajrh2017/v21i3.2.
Aggarwal S, Upadhyay A, Shah D, Teotia N, Agarwal A, Jaiswal V. Lactobacillus GG for treatment of acute childhood diarrhoea: an open labelled, randomized controlled trial. Indian J Med Res. 2014 Mar;139(3):379-85.
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


