Analysis of D-Dimer Levels among Covid -19 Positive Patients in a Tertiary Care Hospital in Bangalore
Abstract
Introduction: Pro-thrombotic changes are stimulated by Corona Virus as it has an affinity for endothelium and lung structures and this may explain its association with thrombotic events, reduction of pulmonary gas exchange, respiratory distress, and death. D-dimer is a specific marker of the breakdown of a fibrin clot and has been used as a diagnostic and prognostic marker in VTE and other coagulation disorders.
Objectives: The objective of this study was to assess the correlation of the D-Dimer levels and disease severity among COVID-19 patients.
Materials and methods: This is a retrospective study done over 6 months from July 2020 to December 2020 in a tertiary care hospital in Bangalore. All the COVID- 19 positive cases who were admitted to our hospital were audited regarding the D-dimer levels during admission and the course of the treatment.
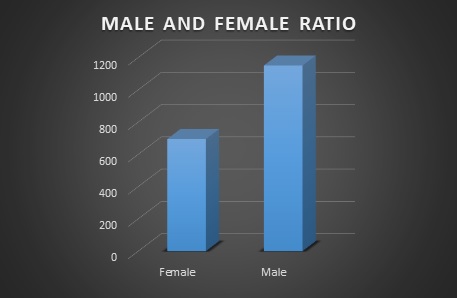
Results: Coagulation disorder occurred at the early stage of COVID-19 infection, with 1066 (57.7%) patients having increased D-dimer levels. Out of 1846 COVID 19 patients 106 (5.7%)patients died due to complications. 106 patients who deceased, all the patients had an increased D dimer value either in the first lab test or in the consecutive tests. Among 106 patients 56(52.8%) patients had increased D-dimer at the first lab test, 32 (30.1%) had D-dimer increased at the second and 18(16.98%) in third lab tests. The increased D-dimer levels were closely associated with the progression of the disease and also the changes in the CT imaging.
Conclusion: The increase in D-Dimer levels also increased the complications in the COVID-19 patient. So it is necessary to continuously monitor D-dimer levels and labelled anticoagulation as management tools for COVID-19 disease to prevent complications and reduce interventions.
Downloads
References
Adam SS, Key NS, Greenberg CS. D-dimer antigen: current concepts and prospects". Blood. 2009;113 (13): 2878–87. doi:10.1182/blood-2008-06-165845.
Kogan AE, Mukharyamova KS, Bereznikova AV, Filatov VL, Koshkina EV, Bloshchitsyna MN, Katrukha AG. Monoclonal antibodies with equal specificity to D-dimer and high-molecular-weight fibrin degradation products". Blood Coagulation & Fibrinolysis. 2016;27 (5): 542–50. doi:10.1097/MBC.0000000000000453.
Olson JD, Cunningham MT, Higgins RA, Eby CS, Brandt JT. D-dimer: simple test, tough problems. Archives of Pathology & Laboratory Medicine. 2013; 137 (8): 1030–8. doi:10.5858/arpa.2012-0296-CP.
Wan Y, Shang J, Graham R, Baric RS, Li F. Receptor Recognition by the Novel Coronavirus from Wuhan: an Analysis Based on Decade-Long Structural Studies of SARS Coronavirus. J Virol. 2020 Mar 17;94(7):e00127-20. doi: 10.1128/JVI.00127-20. PMID: 31996437; PMCID: PMC7081895.
Kowalczuk S, Bröer A, Tietze N, Vanslambrouck JM, Rasko JE, Bröer S. A protein complex in the brush-border membrane explains a Hartnup disorder allele. FASEB J. 2008 Aug;22(8):2880-7. doi: 10.1096/fj.08-107300. Epub 2008 Apr 18. PMID: 18424768.
Cohen J. The immunopathogenesis of sepsis. Nature. 2002 Dec 19-26;420(6917):885-91. doi: 10.1038/nature01326. PMID: 12490963.
Giannitsis E, Mair J, Christersson C, Siegbahn A, Huber K, Jaffe AS, Peacock WF, Plebani M, Thygesen K, Möckel M, Mueller C, Lindahl B; Biomarker Study Group of the European Society of Cardiology (ESC) Acute Cardiovascular Care Association (ACCA). How to use D-dimer in acute cardiovascular care. Eur Heart J Acute Cardiovasc Care. 2017 Feb;6(1):69-80. doi: 10.1177/2048872615610870. Epub 2016 Sep 22. PMID: 26450781.
Ramana CV, DeBerge MP, Kumar A, Alia CS, Durbin JE, Enelow RI. Inflammatory impact of IFN-γ in CD8+ T cell-mediated lung injury is mediated by both Stat1-dependent and -independent pathways. Am J Physiol Lung Cell Mol Physiol. 2015 Apr 1;308(7):L650-7. doi: 10.1152/ajplung.00360.2014. Epub 2015 Jan 23. PMID: 25617378; PMCID: PMC4385989.
Behrens K, Alexander WS. Cytokine control of megakaryopoiesis. Growth Factors. 2018 Aug;36(3-4):89-103. doi: 10.1080/08977194.2018.1498487. Epub 2018 Oct 15. PMID: 30318940.
Liu Y, Gayle AA, Wilder-Smith A, Rocklöv J. The reproductive number of COVID-19 is higher compared to SARS coronavirus. J Travel Med. 2020 Mar 13;27(2):taaa021. doi: 10.1093/jtm/taaa021. PMID: 32052846; PMCID: PMC7074654.
Guan WJ, Ni ZY, Hu Y, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708-1720. doi:10.1056/NEJMoa2002032
Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18(4):844–847. doi: 10.1111/jth.14768.
Chong PY, Chui P, Ling AE, et al. Analysis of deaths during the severe acute respiratory syndrome (SARS) epidemic in Singapore: challenges in determining a SARS diagnosis. Arch Pathol Lab Med. 2004;128(2):195–204.
Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420–422. doi: 10.1016/S2213-2600(20)30076-X.
Lang Z, Zhang L, Zhang S, Meng X, Li J, Song C, Sun L, Zhou Y. Pathological study on severe acute respiratory syndrome. Chin Med J Peking. 2003;07:17–21.
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


