Effectiveness of underlay myringoplasty in inactive mucosal chronic otitis media; a prospective study
Abstract
Introduction: Patients with a mucosal type of chronic otitis media (COM) usually have recurrent ear discharge and conductive hearing loss. It is characterized by the central perforation of the tympanic membrane. Myringoplasty is an operation performed to repair tympanic membrane perforation when there is no ossicular damage. It helps to prevent ear discharge and improves hearing. Different techniques used for myringoplasty are underlay and overlay. Underlay technique is an effective procedure for tympanic membrane repair.
Methods: 125 patients who underwent underlay myringoplasty over two years in a tertiary care center in Kerala were included in the study. Patients with actively discharging ears were excluded from the study.
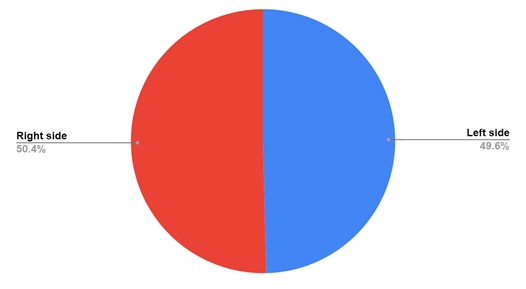
Results: The majority of the patients were in the age group of 20-29 years (49.6%). There were 47 males (37.6%) and 78 females (62.4%). In 63 patients the surgery was done on the right side (50.4%) and in 62 patients on the left side (49.6%). Maximum preoperative hearing loss was in the range of 30-34 dB (39.2%). 100 patients (80%) showed successful graft uptake with the improvement of hearing in the range of 10-15 dB. Eight patients (6.4%) showed small residual perforation with the improvement of hearing. In 17 patients (13.6%) there was a complete rejection of graft with continuous ear discharge and no improvement in hearing.
Conclusion: Underlay myringoplasty is an effective surgical technique for the repair of tympanic membrane perforations in terms of graft take up and improvement of hearing.
Downloads
References
Michael G, Ray C, editors. Scott-Brown's otorhinolaryngology: head and neck surgery. 7th edition, vol. 3 London: CRC Press; 2008. doi: 10.1308/147870811X598605b.
Sergi B, Galli J, De Corso E, Parrilla C, Paludetti G. Overlay versus underlay myringoplasty: report of outcomes considering closure of perforation and hearing function. Acta Otorhinolaryngol Ital. 2011;31(6):366-371.
Gladstone HB, Jackler RK, Varav K. Tympanic membrane wound healing. An overview. Int Arch Otorhinolaryngol.1995;28(5):913-932. doi: 10.1016/S0030-6665(20)30467-9.
Neeta S, Ashwin AJ, Praveer KB, Amrish KG. Complications of chronic suppurative otitis media and their management: A single institution 12 years’ experience. Indian J Otolaryngol Head Neck Surg. 2015;67(4):353-360. doi: 10.1007/s12070-015-0836-5.
Fernandes VLG, Goel HC, De Sousa E, De Gouveia Pinto NM. A comparative study of type-I underlay tympanoplasty with temporalis fascia graft alone and with conchal cartilage. Indian J Otolaryngol Head Neck Surg. 2019;71(2):1320-1326. doi: 10.1007/s12070-018-1397-1.
Liew L, Daudia A, Narula AA. Synchronous fat plug myringoplasty and tympanostomy tube removal in the management of refractory otorrhoea in younger patients. Int J Pediatr Otorhinolaryngol. 2002;66(3):291-296. doi: 10.1016/s0165-5876(02)00257-4.
Aponte RH, Desentis VE, Vargas AA. Factors influencing hearing improvement of patients with chronic otitis media after tympanoplasty, Otorrinolaringología 2007;52(1):22-28. Available at https://www.medigraphic.com/pdfs/anaotomex/aom-2007/aom071f.pdf.
Sarker M, Ahmed M, Patwary K, Islam R, Joarder A. Factors affecting surgical outcome of myringoplasty. Bangladesh J Otorhinolaryngol. 2011;17(2):82-87. doi: 10.3329/bjo.v17i2.8846.
Kripa D, Rakesh PS. Study of various prognostic factors affecting successful myringoplasty in a tertiary care centre. Int Arch Otorhinolaryngol. 2017;21(3):250-254. doi: 10.1055/s-0036-1593818.
Undavalli SB, Kulkarni NH, Bose S, Ananthaneni A. Tympanometric assessment of Eustachian tube function as a prognostic indicator in myringoplasty. Adv Arab Acad Audio-Vestibul J 2017;4(1):14-18. doi: 10.4103/aaaj.aaaj_4_17.
Alam K, Alam MM, Hossain MD, Karim MA, Hossain MA, Sarker MZ. Comparative study of different approaches of myringoplasty in chronic otitis media. Bangladesh J Otorhinolaryngol. 2020;22(1):21-25. doi: 10.3329/bjo.v22i1.45074.
Mahesh SG, Vishwas KP, Pallavi P, Nithin PS. Myringoplasty: underlay versus overlay techniques - a comparative study. Int J Otorhinolaryngol head Neck Surg. 2018;4(2):381-386. doi: 10.18203/issn.2454-5929.ijohns20180697.
Kamath MP, Sreedharan S, Rao AR. et al. Success of myringoplasty: our experience. Indian J Otolaryngol Head Neck Surg. 2013;65(4):358-362. doi: 10.1007/s12070-013-0651-9.
Jyothi AC, Shrikrishna BH, Kulkarni NH, Kumar A. Endoscopic myringoplasty versus microscopic myringoplasty in tubotympanic CSOM: a comparative study of 120 cases. Indian J Otolaryngol Head Neck Surg. 2017;69(3):357-362. doi: 10.1007/s12070-017-1147-9.
Hazem MAT, Fadi MG, Tareq MA, Louay SES. Myringoplasty with and without cortical mastoidectomy in treatment of non-cholesteatomatous chronic otitis media: a comparative study. Clin Med Insights Ear Nose Throat. 2014;7:19-23. doi: 10.4137/CMENT.S17980.
Silviu A, Franco T, and Maurizio A. Usefulness of Cortical Mastoidectomy in Myringoplasty. Otol Neurotol. 2012;33(4):604-609. doi: 10.1097/MAO.0b013e31825368f2.
Razzak MA, Murshed KM, Sobhan A, Hossain MR, Imtiaz SN. Outcome of myringoplasty in underlay technique. Bangladesh J Otorhinolaryngol. 2019;24(2):131-136. doi: 10.3329/bjo.v24i2.44173.
Salmah MA, Wardah YAA, Talat AA, Ali SAQ. Myringoplasty outcome. Five-year experience at a tertiary teaching hospital. Saudi Med J. 2019;40(2):199-201. doi: 10.15537/smj.2019.2.23896
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


