Cardiac evaluation of Covid-19 patients with post-discharge dyspnoea
Abstract
Background: Dyspnoea is one of the common symptoms in COVID-19 patients after discharge from the hospital. So evaluation of cardiac function becomes necessary in COVID patients after hospital discharge.
AIM: To study the cardiac function of COVID 19 patients presenting with dyspnoea after discharge from hospital within 3 months of symptom onset.
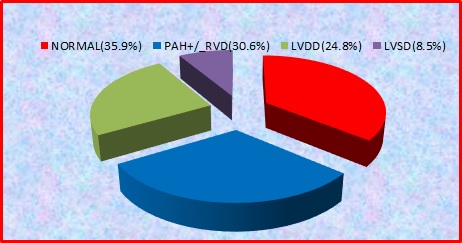
Materials and methods: 245 post-hospital discharge COVID-19 patients enrolled in the study. The patients with abnormal echocardiography are further divided into three groups, A) patients with PAH±RVD, B) patients with LV diastolic dysfunction C) patients with LV systolic dysfunction. Data of the three groups were compared.
Results: Out of 245 patients, 64% (157) patients show abnormal echocardiogram.75 (30.6%) patient show PAH±RVD,61(24.8% ) patients shows LV diastolic dysfunction and 21(8.57%) patients shows LV systolic dysfunction. patients with ventricular dysfunction significantly associated with multiple risk factors and comorbidity. Grade 1,2,3,4 diastolic dysfunction seen in 27.8%,34.4%,29.5%,8.1% in group B respectively. LV systolic dysfunction is mild in 13 (61.9%), moderate in6(28.5%), severe in 1 (4.7 %) in group C patients. Ntprobnp, tropnin significantly higher in all groups. Also, CRP, D dimer significantly higher in group A, but non significantly higher in group B, C.
Conclusion: RV dysfunction is the most common pattern seen in around 30% of patients. LV diastolic dysfunction is not uncommon, seen in ¼ the patients. Patients with cardiac dysfunction have a high level of cardiac and inflammatory biomarkers, which can lead to grievous cardiovascular complications. So close follow up required.
Downloads
References
Hamming I, Timens W, Bulthuis ML, Lely AT, Navis GV, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203(2):631-637. doi:10.1002/path.1570
Potus F, Mai V, Lebret M, Malenfant S, Breton-Gagnon E, Lajoie AC, Boucherat O, Bonnet S, Provencher S. Novel insights on the pulmonary vascular consequences of COVID-19. Am J Physiol-Lung Cell Molecular Physiol. 2020;319(2):L277-L288. doi:10.1152/ajplung.00195.2020.
Wise J. Covid-19: Symptoms are common after acute phase of disease, Italian study shows. doi: 10.1136/bmj.m2804.
Carfì A, Bernabei R. Landi FGemelli Against COVID-19 Post-Acute Care Study Group, for the Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent symptoms in patients after acute Covid-19. JAMA.2020;324(6):603-605. doi:10.1001/jama.2020.12603.
Arcasoy SM, Christie JD, Ferrari VA, Sutton MS, Zisman DA, Blumenthal NP, Pochettino A, Kotloff RM. Echocardiographic assessment of pulmonary hypertension in patients with advanced lung disease. Am J Resp Critical Care Med. 2003;167(5):735-740. doi: 10.1503/erp-17-0071.
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF, Dokainish H, Edvardsen T, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. European J Echocardiograph. 2016;17(12):1321-1360. doi: 10.1016/j.echo.2016.01.011.
Zerbib Y, Maizel J, Slama M. Echocardiographic assessment of left ventricular function. doi: 10.21037/jeccm.2019.07.05.
Szekely Y, Lichter Y, Taieb P, Banai A, Hochstadt A, Merdler I, et al. The Spectrum of Cardiac Manifestations in Coronavirus Disease 2019 (COVID-19)-a Systematic Echocardiographic Study. Circulation. 2020;142(4):342-353. doi: 10.1161/circulationaha.120.047971.
Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052-2059 doi: 10.1001/jama.2020.6775.
Pagnesi M, Baldetti L, Beneduce A, Calvo F, Gramegna M, Pazzanese V, et al. Pulmonary hypertension and right ventricular involvement in hospitalised patients with COVID-19. Heart. 2020;106(17):1324-1331. doi: 10.1136/heartjnl-2020-317355.
Moody WE, Mahmoud-Elsayed HM, Senior J, Gul U, Khan-Kheil AM, Horne S, et al. Impact of Right Ventricular Dysfunction on Mortality in Patients Hospitalized with COVID-19 according to Race. CJC open. 2020. doi: 10.1016?j.cjco.2020.09.016.
Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;5(11):1265-1273. doi: 10.1001/jama cardio.2020.3557.
Bangalore S, Sharma A, Slotwiner A, Yatskar L, Harari R, Shah B, et al. ST-segment elevation in patients with Covid-19—a case series. N Eng J Med. 2020;382(25):2478-2480. doi:10.1056/NEJMc20009020.
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


