A clinico-epidemiological study of the first outbreak of Nipah virus in India – report from ground zero
Abstract
Introduction: The first Nipah Virus (NiV) outbreak occurred in India in the year 2001 at Siliguri. The second outbreak happened at Nadia in 2007. Nipah Virus exhibits neurological and pneumonic tropism with the predominant clinical presentation being encephalitis in humans.
Material and Methods: The present study was a record based prospective study on 67 cases admitted with pyrexia of unknown origin in North Bengal Medical College during the period from 18.02.2001 to 30.02.2001 and a parallel study on epidemiological record carried out by PSM department also taken into account. All necessary investigations including autopsy examination, pathological, and microbiological study were done.
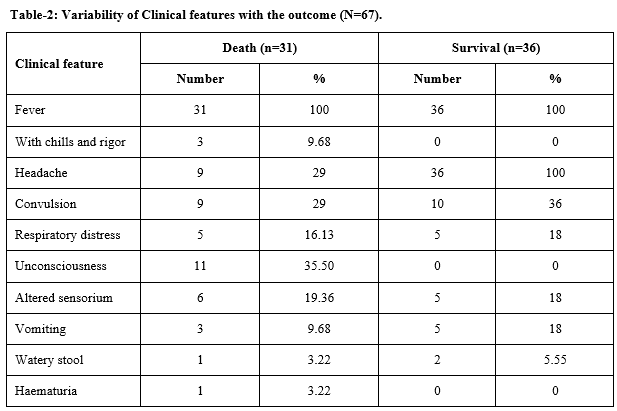
Results: There was a clustering of cases around Bhaktinagar. There was a strong H/O Medinova Nursing Home Contact among the patients. 18 out of 20 cases were staff of that Nursing Home. Serum samples tested show NiV specific IgM and IgG in 9 out of 17 samples with one sample which was positive for IgG only suggesting past infection. The cases were admitted with predominant neurological symptoms (53.73% cases) but about 80% recovered with no residual neuro deficit. The natural reservoir of NiV is present in Bangladesh and in Northern India.
Conclusion: When NiV infection is suspected, infection control practices must be strengthened to avoid an outbreak in a hospital setting. Here the present study is presenting the experience in the first outbreak of the Nipah virus in India at Siliguri for awareness of clinical personnel to control further outbreak at the very beginning.
Downloads
References
Kumar S. Inadequate research facilities fail to tackle mystery disease. BMJ. 2003;326:12. doi: https://doi.org/10.1136/bmj.326.7379.12/d.
Chua KB, Bellini WJ, Rota PA, Harcourt BH, Tamin A, Lam SK, et al. Nipah virus: a recently emergent deadly paramyxovirus. Sci. 2000;288(5470):1432-1415. doi: 10.1126/science.288.5470.1432.
ICDDR B. Nipah encephalitis outbreak over wide area of western Bangladesh, 2004. Health Sci Bullet. 2004;2(1):7-11.
CDDRB Person-to-person transmission of Nipah virus during outbreak in Faridpur District. Health Sci Bullet. 2004;2(2):5-9.
World Health Organization: Nipahvirus outbreak(s) in Bangladesh, January–April 2004. Wkly Epidemiol Rec. 2004;17:168-171. Available at https://apps.who.int/iris/handle/10665/232464.
Hsu VP, Hossain MJ, Parashar UD, Ali MM, Ksiazek TG, Kuzmin I, et al. Nipah virus encephalitis reemergence, Bangladesh. Emerg Infect Dis. 2004;10(12):2082-2087. doi: https://doi.org/10.3201/eid1012.040701.
Goh KJ, Tan CT, Chew NK, Tan PS, Kamarulzaman A, Sarji SA, et al. Clinical features of Nipah virus encephalitis among pig farmers in Malaysia. N Engl J Med. 2000;342:1229-1235. doi: https://doi.org/10.1056/NEJM200004273421701.
Mounts AW, Kaur H, Parashar UD, Ksiazek TG, Cannon D, Arokiasamy JT, et al. Nipah Virus Nosocomial Study Group A cohort study of health care workers to assess nosocomial transmissibility of Nipah virus. J Infect Dis. 2001;183(5):810-813. doi: https://doi.org/10.1086/318822.
Chan KP, Rollin PE, Ksiazek TG, Leo YS, Goh KT, Paton NI, et al. A survey of Nipah virus infection among various risk groups in Singapore. Epidemiol Infect. 2002;128(1):93-98. doi https://doi.org/10.1017/S0950268801006422.
Chadha MS, Comer JA, Lowe L, Rota PA, Rollin PE, Bellini WJ, et al. Nipah Virus-associated Encephalitis Outbreak, Siliguri, India. Emerg Infect Dis. 2006;12(2):235-240. doi: https://doi.org/10.3201/eid1202.051247.
Reynes JM, Counor D, Ong S, Faure C, Seng V, Molia S, et al. Nipah Virus in Lyle's flying foxes, Cambodia. Emerg Infect Dis. 2005;11(7):1042-1047. doi: https://doi.org/10.3201/eid1107.041350.
Yob JM, Field H, Rashdi AM, Morrissy C, van der Heide B, Rota P, et al. Nipah virus infection in bats (orderChiroptera) in peninsular Malaysia. Emerg Infect Dis. 2001;7(3):439-441. doi: https://doi.org/10.3201/eid0703.010312.
Ang BSP, Lim CCT , Wang L. Nipah Virus Infection. J Clini Microbiol. 2018;56(6):1875-1817. doi: https://doi.org/10.1128/JCM.01875-17.
Looi LM, Chua KB. Lessons from the Nipah virus outbreak in Malaysia. Malays J Pathol. 2007;29(2):63-67.
Ang BS, Lim TC, Wang L. Nipah virus infection. J Clin Microbiol. 2018;56(6):e01875-17. doi: https://doi.org/10.1128/JCM.01875-17.
Hossain MJ, Gurley ES, Montgomery JM, Bell M, Carroll DS, Hsu VP, et al. Clinical presentation of Nipah virus infection in Bangladesh. Clin Infect Dis. 2008;46(7):977-984. doi: https://doi.org/10.1086/529147.
Chadha MS, Comer JA, Lowe L, Rota PA, Rollin PE, Bellini WJ, et al. Nipah virus-associated encephalitis outbreak, Siliguri, India. Emerg Infect Dis. 2006;12(2):235-240. doi: https://doi.org/10.3201/eid1202.051247.
Mandal S, Banerjee R. Bat Virus in Bengal. The Telegraph. 2007. Available at https://www.telegraphindia.com/india/bat-virus-in-bengal/cid/707729.
Luby SP, Gurley ES, Hossain MJ. Transmission of human infection with Nipah virus. Clin Infect Dis. 2009;49(11):1743-1748. doi: https://doi.org/10.1086/647951.
Hahn MB, Epstein JH, Gurley ES, Islam MS, Luby SP, Daszak P, et al. Roosting behaviour and habitat selection of Pteropusgiganteus reveals potential links to Nipah virus epidemiology. J Appl Ecol. 2014;51(2):376-387. doi: https://doi.org/10.1111/1365-2664.12212.
Ching PK, de los Reyes VC, Sucaldito MN, Tayag E, Columna-Vingno AB, Malbas FF., Jr Outbreak of henipavirus infection, Philippines, 2014. Emerg Infect Dis. 2015;21(2):328-331. doi: https://doi.org/10.3201/eid2102.141433.
KumarA. K; KumarA. S. Deadly Nipah Outbreak in Kerala: Lessons Learned for the Future. Indian J Crit Care Med. 2018;22(7):475-476. doi: https://doi.org/10.4103/ijccm.IJCCM_282_18.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


