Clinical profile and outcome of organophosphorus poisoning in a tertiary care centre, a prospective observational study
Abstract
Introduction: Acute organophosphorus (OP) pesticide poisoning is widespread in the developing world. Being predominantly an agricultural country, pesticides and insecticides are used abundantly for cultivation, and access to these poisonous chemical substances by the population is easy. The objectiveof the study was to identifythe nature of the demographic profile, type of compound, clinical manifestations, and outcome of organophosphate poisoning presenting to a tertiary care teaching hospital in India.
Material and methods: A cross-sectional study was conducted among 100 patients admitted with OPC poisoning inthe department of general medicine,Velammal Medical College Hospital and Research Institute, Madurai from January 2016 to July 2019. The diagnosis was made based on history or evidence of exposure to OP compound within 24 hours; characteristic manifestations of OP poisoning include, miosis, fasciculations, excessive salivation, improvement of signs and symptoms with administration of atropine were recorded. IBM SPSS version 22 was used for statistical analysis.
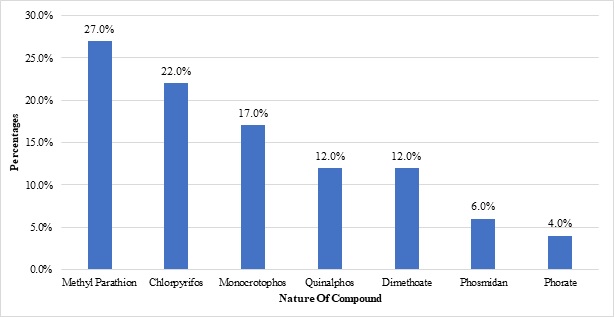
Results:The majority of the subjects were males(80%). The majority (66%) were in the age group of 21-40 years. The most common OPC to be consumed was Methyl parathion (27%), followed by chlorpyrifos (22%). The major GIT complications were abdominal pain/cramps (100%), followed by nausea and vomiting (83%). Mechanical ventilation was needed in 40% and mortality was reported in 25% of the subjects.
Conclusion:OP poisoning affects resonantly males in their economically productive phase of life. Considering the high mortality, adequate strengthening of health services, especially at the primary level is the need of the hour.
Downloads
References
Unnikrishnan B, Singh B, Rajeev A. Trends of acute poisoning in south Karnataka. Kathmandu Univ Med J. 2005;3(2):149-154.
Accidental deaths and suicides in India National Crime Records Bureau Ministry of Home affairs Government of India. National Crime Records Bureau, Ministry of Home affairs, Government of India. 2017. Available from: http://ncrb.gov.in/.
Sharma B, Harish D, Sharma V, Vij K. The epidemiology of poisoning: An Indian view point. J Foren Med Toxicol. 2002;19(2):5-11.
Behere PB, Behere AP. Farmers' suicide in Vidarbha region of Maharashtra state: A myth or reality? Indian J Psychiatry. 2008;50(2):124-127. doi: https://dx.doi.org/10.4103/0019-5545.42401.
Zawar S. Correlation between plasma cholinesterase levels and clinical severity of acute organophosphate and carbamate poisoning. JAPI. 2001;149:91.
Aygun D, Doganay Z, Altintop L, Guven H, Onar M, Deniz T, et al. Serum acetylcholinesterase and prognosis of acute organophosphate poisoning. J Toxicol: Clin Toxicol. 2002;40(7):903-910. doi: https://doi.org/10.1081/clt-120016962.
Banerjee I, Tripathi S, Roy AS. Clinico-epidemiological characteristics of patients presenting with organophosphorus poisoning. N Am J Med Sci. 2012;4(3):147-150. doi: https://dx.doi.org/10.4103/1947-2714.93884.
Cherian M, Roshini C, Visalakshi J, Jeyaseelan L, Cherian A. Biochemical and clinical profile after organophosphorus poisoning A placebo controlled trial using pralidoxime. J Assoc Physicians India. 2005;53:427-431.
Banday TH, Tathineni B, Desai MS, Naik V. Predictors of Morbidity and Mortality in Organophosphorus Poisoning: A Case Study in Rural Hospital in Karnataka, India. N Am J Med Sci. 2015;7(6):259-265. doi: https://dx.doi.org/10.4103/1947-2714.159331.
Khan S, Kumar S, Agrawal S, Bawankule S. Correlation of serum cholinesterase and serum creatine phosphokinase enzymes with the severity and outcome of acuteorganophosphorus poisoning: study in rural central India. World J Pharmacy Pharmac Sci. 2016;5(4):1365-1373. doi: https://dx.doi.org/10.20959/wjpps20164-6389.
Chintale KN, Patne SV, Chavan SS. Clinical profile of organophosphorus poisoning patients at rural tertiary health care centre. Int J Adv Med. 2016;3(2):268-274. doi: https://dx.doi.org/10.18203/2349-3933.ijam20161074.
Noshad H, Ansarin K, Ardalan MR, Ghaffari AR, Safa J, Nezami N. Respiratory failure in organophosphate insecticide poisoning. Saudi Med J. 2007;28(3):405-407.
Singhal A, Yang M, Sargent M, Cochrane D. Does optic nerve sheath diameter on MRI decrease with clinically improved pediatric hydrocephalus?. Child's Nerv Syst. 2012;29(2):269-279. doi: https://dx.doi.org/10.1007/s00381-012-1937-z
Rao GV,JyothsnaM. Relation between Serum Cholinesterase and Mortality among Patients with OP Poisoning. Indian J Clin Anaesth. 2016;3(1):48-51.
Sungur M, Guven M. Intensive care management of organophosphate insecticide poisoning. Crit Care. 2001;5(4):211-215. doi: https://dx.doi.org/10.1186%2Fcc1025.
Shah SM, Asari PD, Amin AJ. Clinico-epidemiological profile of patients presenting with acute poisoning. Int J Curr Res Rev. 2016;8(13):35-41.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


