Pattern recognition approach and clinico-radiological evaluation of compressive myelopathies at a tertiary care hospital
Abstract
Background: Neuroimaging is indicated in most instances of new-onset myelopathy for clinico-radiological correlation in terms of diagnosis, recovery, and prediction of recurrence.
Aim: This study was conducted to study the clinical profile of cases of Compressive Myelopathy and the pattern of spinal cord involvement, also to compare the sites of localisation of clinical diagnosis with MRI diagnosis. Methodology: The present study was a prospective study involving 30 patients. Patients with clinical suspicion of spinal cord disease of age group 20-80 years were included as study participants. The primary pulse sequences included T1 and T2 weighted images on MRI, the location of the lesion, its margins, signal intensity on both T1 and T2 weighted images was noted.
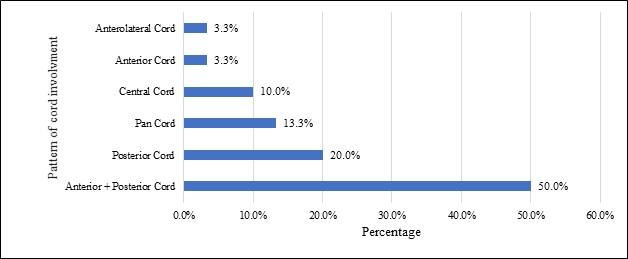
Results: The majority of 53.33% of participants were aged between 51 to 60 years. Difficulty in walking was observed in 97% of participants. Men were more often affected than women. Cervical spondylosis was the commonest cause of compressive myelopathy in 57%. A most common pattern of spinal cord involvement was combined Anterior + Posterior cord involvement. The cervical site of localisation (54%) was the commonest followed by the thoracic and lumbar spinal cord.
Conclusion: Myelopathies have male preponderance. The commonest cause of compressive myelopathy was Cervical spondylosis. Anterior plus posterior cord syndrome was the commonest pattern seen, followed by posterior cord syndrome, anterior cord syndrome being the least observed. MRI correlates well with a clinical diagnosis and is useful in suggesting the location of the lesion.
Downloads
References
Mariano R, Flanagan EP, Weinshenker BG, Palace J. A practical approach to the diagnosis of spinal cord lesions. Pract Neurol. 2018;18(3):187-200. doi: https://doi.org/10.1136/practneurol-2017-001845.
Seidenwurm DJ, Expert Panel on Neurologic I. Myelopathy. AJNR Am J Neuroradiol. 2008;29(5):1032-1034.
Rothman MI, Zoarski GH, Akhtar N. Extradural causes of myelopathy. Semin Ultrasound CT MR. 1994;15(3):226-249. doi: https://doi.org/10.1016/s0887-2171(05)80073-3.
Fehlings MG, Tetreault LA, Riew KD, Middleton JW, Aarabi B, Arnold PM, et al. A Clinical Practice Guideline for the Management of Patients With Degenerative Cervical Myelopathy: Recommendations for Patients With Mild, Moderate, and Severe Disease and Nonmyelopathic Patients With Evidence of Cord Compression. Global Spine J. 2017;7(3):70S-83S. doi: https://doi.org/10.1177/2192568217701914.
Fehlings MG, Tetreault L, Nater A, Choma T, Harrop J, Mroz T, et al. The Aging of the Global Population: The Changing Epidemiology of Disease and Spinal Disorders. Neurosurg. 2015;77(4):S1-S5. doi: https://doi.org/10.1227/NEU.0000000000000953.
McCormick WE, Steinmetz MP, Benzel EC. Cervical spondylotic myelopathy: make the difficult diagnosis, then refer for surgery. Cleve Clin J Med. 2003;70(10):899-904. doi: http://doi.org/10.3949/ccjm.70.10.899.
Klineberg E. Cervical spondylotic myelopathy: a review of the evidence. Orthop Clin North Am. 2010;41(2):193-202. doi: https://doi.org/10.1016/j.ocl.2009.12.010.
Marquis BO, Capone PM. Chapter 52 - Myelopathy. Handbook of Clinical Neurology. 136: Elsevier; 2016. p. 1015-1026.
Wong SH, Boggild M, Enevoldson TP, Fletcher NA. Myelopathy but normal MRI: where next? Pract Neurol. 2008;8(2):90-102. doi: https://doi.org/10.1136/jnnp.2008.144121.
IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.
Granados S, Ana M, Garcia P, Lina M, Ortega T, Cesar A, et al. Diagnostic approach to myelopathies. Revista Colombiana de Radiología. 2011;22(3):3231-3251.
Gay CW, Bishop MD, Beres JL. Clinical presentation of a patient with thoracic myelopathy at a chiropractic clinic. J Chiropr Med. 2012;11(2):115-120. doi: https://doi.org/10.1016/j.jcm.2011.10.007.
Sarathchand V, Sambasivarao K, Anuradha B, Sudharani B. Role of MRI in the Evaluation of Compressive Myelopathy. OSR J Dent Med Sci. 2016;15(4):21-26. doi: https://doi.org/10.9790/0853.1504132126.
Haleem MA, Islam MS, Quraishi F, Hossain S, Gosh L, Wadud MS, Mohammed Shoab A. Magnetic Resonance Imaging-Based Evaluation of the Etiology of Non-Traumatic Myelopathies in Bangladesh: A Hospital-based Observational Cross-sectional Study from Two Tertiary Care Centers of Dhaka. JNINB. 2020;4(2):87-91. doi: https://doi.org/10.3329/jninb.v4i2.38920.
Fidele NJ, Amanuel A. Spectrum of nontraumatic myelopathies in Ethiopian patients: hospital-based retrospective study. Spinal Cord. 2016;54(8):604-608. doi: https://doi.org/10.1038/sc.2015.226.
Northover JR, Wild JB, Braybrooke J, Blanco J. The epidemiology of cervical spondylotic myelopathy. Skeletal Radiol. 2012;41(12):1543-1546. doi: https://doi.org/10.1007/s00256-012-1388-3.
Faysal MM, Sutradhar SR, Saha SK, Nuary N, Hosen MA, Talukder RK, et al. Aetiology of Myelopathy in a Tertiary Hospital of Bangladesh. Mymensingh Med J. 2019;28(2):268-273.
Malone A, Meldrum D, Bolger C. Gait impairment in cervical spondylotic myelopathy: comparison with age- and gender-matched healthy controls. Eur Spine J. 2012;21(12):2456-66. doi: https://doi.org/10.1007/s00586-012-2433-6.
Kumar PS, Kalpana RY. Clinico-radiological correlation in a cohort of cervical myelopathy patients. J Clin Diagn Res. 2015;9(1):TC01-TC07. doi: https://doi.org/10.7860/JCDR/2015/10850.5378.
Ann M, Henwood H. Cervical spondylosis with myelopathy: painful and sometimes paralyzing. Am Nurse Today. 2011;6:6.
Nishimura H, Endo K, Suzuki H, Tanaka H, Shishido T, Yamamoto K. Gait Analysis in Cervical Spondylotic Myelopathy. Asian Spine J. 2015;9(3):321-6. doi: https://doi.org/10.4184/asj.2015.9.3.321.
Okada S, Chang C, Chang G, Yue JJ. Venous hypertensive myelopathy associated with cervical spondylosis. Spine J. 2016;16(11):e751-e754. doi: https://doi.org/10.1016/j.spinee.2016.06.003.
Matsunaga S, Komiya S, Toyama Y. Risk factors for development of myelopathy in patients with cervical spondylotic cord compression. Eur Spine J. 2015;24(2):142-149. doi: https://doi.org/10.1007/s00586-013-2839-9.
Wang SQ, Li X, Cui JL, Li HX, Luk KD, Hu Y. Prediction of myelopathic level in cervical spondylotic myelopathy using diffusion tensor imaging. J Magn Reson Imaging. 2015;41(6):1682-1688. doi: https://doi.org/10.1002/jmri.24709.
Haleem MA, Islam MS, Quraishi FA, Hossain S, Gosh L, Wadud MS, et al. Magnetic Resonance Imaging-Based Evaluation of the Etiology of Non-Traumatic Myelopathies in Bangladesh: A Hospital-based Observational Cross-sectional Study from Two Tertiary Care Centers of Dhaka. J Nat Instit Neurosci Bangladesh. 2018;4(2):87-91. doi: https://doi.org/10.3329/jninb.v4i2.38920.
Lavelle WF, Bell GR. Cervical myelopathy: history and physical examination. Seminars in Spine Surgery. 19: Elsevier; 2007. p. 6-11.
Boogaarts HD, Bartels RH. Prevalence of cervical spondylotic myelopathy. Eur Spine J. 2015;24(2):139-141. doi: https://doi.org/10.1007/s00586-013-2781-x.
Erdal Y, Emre U, Darliance ZS, Lean OÖ, Kılıçkesmez NÖ. Myelopathy: Retrospective Evaluation of Twenty-Eight Cases. Turk J Norol. 2017;23(4):186-192.
Gupta RK, Agarwal P, Kumar S, Surana PK, Lal JH, Misra UK. Compressive myelopathy in fluorosis: MRI. Neuroradiol. 1996;38(4):338-342. doi: https://doi.org/10.1007/bf00596584.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


