Comparative evaluation of continuous epidural infusion of 0.0625% Bupivacaine + 0.0002% Fentanyl and 0.1% Ropivacaine + 0.0002% Fentanyl for labour analgesia
Abstract
Aim& Objectives: To compare the total dose of Fentanyl and Bupivacaine with total dose of Ropivacaine and fentanyl in terms of total volume delivered-loading, infusion and top ups. Also, to compare Analgesic efficacy (VAS score) and adverse events if any.
Methods: 60 ASA physical status I or II parturients in labour who were either primigravidae or gravida 2 were included in a randomized, single blind, prospective study. After a bolus dose of 0.125 % Bupivacaine and 25 mcg Fentanyl, the group BF received a continuous epidural infusion of 0.0625% Bupivacaine and 0.0002% Fentanyl whereas the group RF received a bolus of 0.2% Ropivacaine and 25 mcg Fentanyl followed by an infusion of 0.1% Ropivacaine and 0.0002% Fentanyl.
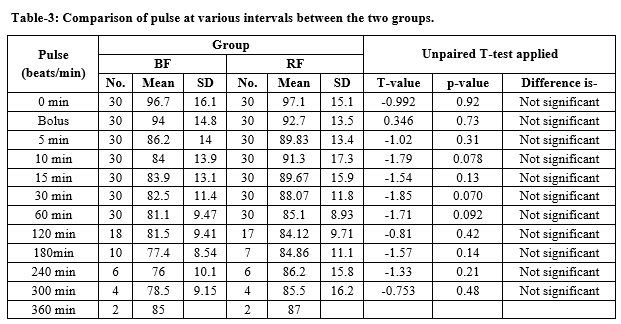
Results: The Group BF and Group RF were comparable with respect to their physical parameters. It was seen that the pain relief in the group BF was excellent for 8 out of 30 patients (26.67%) whereas for the group RF it was excellent for 9 of 30 patients (30%). After that till delivery, both the groups had a comparable mean maternal pulse rate (p value >0.05). None of the parturient in study or control group ever had an episode of bradycardia. Throughout the remaining period of analgesia, the mean foetal heart rate was comparable between the two groups. In the present study groups only 2 parturients from group BF and only one parturient from group RF underwent caesarean section due to foetal distress. 6 parturients (20%) from group BF and 5 parturients (16.67%) from group RF developed hypotension.
Conclusion: Continuous infusion of 0.1% Ropivacaine + 0.0002 % Fentanyl provides equipotent labour analgesia and maternal satisfaction as 0.0625% Bupivacaine + 0.0002% Fentanyl infusion can provide.
Downloads
References
Taneja B, Nath K, Dua CK. Clinical audit on the existing attitudes and knowledge of obstetricians regarding labour analgesia. Indian J Anaesth. 2004;48(3):185-188.
Reynolds F. The effects of maternal labour analgesia on the fetus. Best Prac Res Clinic Obstet Gynaecol. 2010;24(3):289-302. doi: https://doi.org/10.1016/j.bpobgyn.2009.11.003.
Cambic CR, Wong CA. Labour analgesia and obstetric outcomes. Brit J Anaesthes. 2010;105(1):i50-60. doi: https://doi.org/10.1093/bja/aeq311.
Saravanakumar K, Garstang JS, Hasan K. Intravenous patient-controlled analgesia for labour: a survey of UK practice. Int J Obstet Anesthes. 2007;16(3):221-225. doi: https://doi.org/10.1016/j.ijoa.2007.01.010.
James JN, Prakash KS, Ponniah M. Awareness and attitudes towards labour pain and labour pain relief of urban women attending a private antenatal clinic in Chennai, India. Indian J Anaesth. 2012;56(2):195-198. doi: https://dx.doi.org/10.4103%2F0019-5049.96331.
Shidhaye RV, Galande MV, Bangal VB, Joshi SS, Shidhaye UR. Awareness and attitude towards labour analgesia of Indian pregnant women. Anaesth Pain & Intensive Care. 2012;16(2):131-6.
Othman M, Jones L, Neilson JP. Non‐opioid drugs for pain management in labour. Cochrane Data System Rev. 2012(7). doi: https://doi.org/10.1002/14651858.CD009223.pub2.
Van der Vyver M, Halpern S, Joseph G. Patient-controlled epidural analgesia versus continuous infusion for labour analgesia: a meta-analysis. Brit J Anaesthes. 2002;89(3):459-465. doi: https://doi.org/10.1093/bja/aef217.
Tveit TO, Seiler S, Halvorsen A, Rosland JH. Labour analgesia: a randomised, controlled trial comparing intravenous remifentanil and epidural analgesia with ropivacaine and fentanyl. Europe J Anaesthesiol (EJA). 2012;29(3):129-136. doi: https://doi.org/10.1097/EJA.0b013e32834dfa98.
Patkar CS, Vora K, Patel H, Shah V, Modi MP, Parikh G. A comparison of continuous infusion and intermittent bolus administration of 0.1% ropivacaine with 0.0002% fentanyl for epidural labor analgesia. J Anaesthesiol, Clinic Pharmacol. 2015;31(2):234-238. https://doi.org/10.4103/0970-9185.155155
Fernández-Guisasola J, Serrano ML, Cobo B, Muñoz L, Plaza A, Trigo C, del Valle SG. A comparison of 0.0625% bupivacaine with fentanyl and 0.1% ropivacaine with fentanyl for continuous epidural labor analgesia. Anesthes & Analg. 2001;92(5):1261-1265. doi: https://doi.org/10.1097/00000539-200105000-00034.
Li Y, Hu C, Fan Y, Wang H, Xu H. Epidural analgesia with amide local anesthetics, bupivacaine, and ropivacaine in combination with fentanyl for labor pain relief: a meta-analysis. Med Sci Monit. 2015; 21: 921–928. doi: https://dx.doi.org/10.12659%2FMSM.892276.
Lee BB, Kee WD, Lau WM, Wong AS. Epidural infusions for labor analgesia: a comparison of 0.2% ropivacaine, 0.1% ropivacaine, and 0.1% ropivacaine with fentanyl. Reg Anesth Pain Med. 2002;27(1):31-36. doi: https://doi.org/10.1053/rapm.2002.27836.
Wang LZ, Chang XY, Xia LI, Hu XX, Tang BL. Comparison of bupivacaine, ropivacaine and levobupivacaine with sufentanil for patient-controlled epidural analgesia during labor: a randomized clinical trial. Chinese Med J. 2010;123(2):178-183.
Sultan P, Murphy C, Halpern S, Carvalho B. The effect of low concentrations versus high concentrations of local anesthetics for labour analgesia on obstetric and anesthetic outcomes: a meta-analysis. Canad J Anesthes. 2013;60(9):840-854. doi: https://doi.org/10.1007/s12630-013-9981-z.
Lee BB, Kee WD, Ng FF, Lau TK, Wong EL. Epidural infusions of ropivacaine and bupivacaine for labor analgesia: a randomized, double-blind study of obstetric outcome. Anesthes Analg. 2004;98(4):1145-1152. doi: https://doi.org/10.1213/01.ane.0000103264.71747.0f.
Impey L, MacQuillan K, Robson M. Epidural analgesia need not increase operative delivery rates. Am J Obstet Gynecol. 2000;182(2):358-363. doi: https://doi.org/10.1016/s0002-9378(00)70224-9.
Congedo E, Sgreccia M, De Cosmo G. New drugs for epidural analgesia. Curr Drug Targets. 2009;10(8):696-706. doi: https://doi.org/10.2174/138945009788982441.
Drysdale SM, Muir H. New techniques and drugs for epidural labor analgesia. Sem Perinatol. 2002;26(2):99-108. doi: https://doi.org/10.1053/sper.2002.32202.
Wong CA. Advances in labor analgesia. Int J Womens Health. 2009;1:139-154. doi: https://dx.doi.org/10.2147%2Fijwh.s4553.
Pandya ST. Labour analgesia: Recent advances. Indian J Anaesth. 2010;54(5):400-408. doi: https://dx.doi.org/10.4103%2F0019-5049.71033.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


