Factors associated with poor outcome in tuberculous meningitis; study from a tertiary care referral Centre from South India
Abstract
Introduction: Tuberculosis (TB) remains a worldwide burden with a large majority of new active cases occurring in underdeveloped and developing countries. This study is an attempt to look into various aspects of the disease that can be associated with the outcome, to promote a timely referral to an appropriate centre. Purpose: To identify various clinical, lab, CSF and radiological variables associated with poor outcome of TBM at the time of discharge.
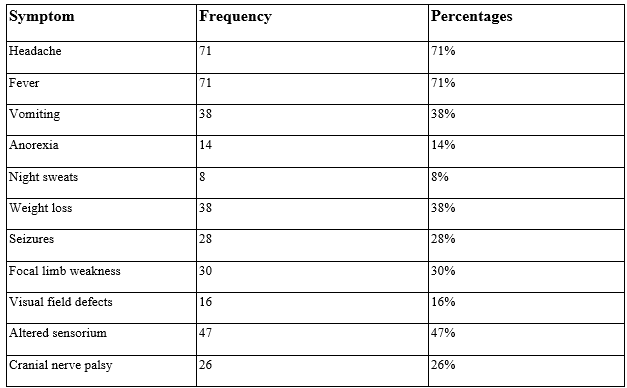
Material & Methods: Demographic data, duration of symptoms before diagnosis, clinical presentation, staging of the disease at the time of admission of all the TBM patients who presented to our centre between December, 2015 and May 2018 were noted. Results of biochemical investigations and brain and spine imaging were retrieved. Outcome at the time of discharge as measured by MRC and mRS grades was correlated to clinical profile, lab, CSF and radiological findings.
Results: A total of 100 patients were included. 15 patients died. Subjects with MRC and mRS grades of 2 or more at admission constituted 65% and 93% respectively. At discharge, MRC and mRS grades of 2 or more were found in 29.63% and 39% respectively. Multivariable analysis showed a significant positive association of MRC stage at discharge with MRC stage (p = 0.001) and mRS score (p = 0.001) at admission and Vellore hydrocephalus grade (p < 0.001) when hydrocephalus first identified. Similarly, mRS score at discharge had an independent positive association with the MRC stage (p < 0.001) and the mRS score (p=0.002) at admission.
Conclusion: Stage of the disease (MRC) and functional status of the patient (mRS) at admission are the two most important independent factors determining the outcome of TBM patients at the time of discharge.
Downloads
References
Van TT, Farrar J. Tuberculous meningitis. J Epidemiol Community Health. 2014 Mar;68(3):195-6. doi: 10.1136/jech-2013-202525.
WHO. Global tuberculosis report: the burden of disease caused by TB. WHO/HTM/TB/2013.11. Geneva, Switzerland: World Health Organization; 2013.
WHO. Global tuberculosis control: WHO report 2016. report. Geneva: World Health Organization, 2016.
George EL, Iype T, Cherian A, Chandy S, Kumar A, Balakrishnan A, Vijayakumar K. Predictors of mortality in patients with meningeal tuberculosis. Neurol India. 2012 Jan-Feb;60(1):18-22. doi: 10.4103/0028-3886.93583.
Misra UK, Kalita J, Srivastava M, Mandal SK. Prognosis of tuberculous meningitis: a multivariate analysis. J Neurol Sci. 1996 Apr;137(1):57-61. doi: 10.1016/0022-510x(95)00334-x.
Thwaites GE, Tran TH. Tuberculous meningitis: many questions, too few answers. Lancet Neurol. 2005 Mar;4(3):160-70. doi: 10.1016/S1474-4422(05)01013-6.
Chakraborty, A. K. "Estimating mortality from tuberculous meningitis in a community: use of available epidemiological parameters in the Indian context." Indian Journal of Tuberculosis 47.1 (2000): 9-13.
Thwaites GE, Nguyen DB, Nguyen HD, Hoang TQ, Do TT, Nguyen TC, et al. Dexamethasone for the treatment of tuberculous meningitis in adolescents and adults. N Engl J Med. 2004 Oct 21;351(17):1741-51. doi: 10.1056/NEJMoa040573.
Kalita J, Misra UK, Ranjan P. Predictors of long-term neurological sequelae of tuberculous meningitis: a multivariate analysis. Eur J Neurol. 2007 Jan;14(1):33-7. doi: 10.1111/j.1468-1331.2006.01534.x. Erratum in: Eur J Neurol. 2007 Mar;14(3):357.
IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.
Cherian A, Thomas SV. Central nervous system tuberculosis. Afr Health Sci. 2011 Mar;11(1):116-27.
Verdon R, Chevret S, Laissy JP, Wolff M. Tuberculous meningitis in adults: review of 48 cases. Clin Infect Dis. 1996 Jun;22(6):982-8. doi: 10.1093/clinids/22.6.982.
Kent SJ, Crowe SM, Yung A, Lucas CR, Mijch AM. Tuberculous meningitis: a 30-year review. Clin Infect Dis. 1993 Dec;17(6):987-94. doi: 10.1093/clinids/17.6.987.
A. R. Rich and H. A. McCordock. The pathogenesis of tuberculous meningitis. Bulletin of the Johns Hopkins Hospital, vol. 52, pp. 5–37, 1933.
Hsu PC, Yang CC, Ye JJ, Huang PY, Chiang PC, Lee MH. Prognostic factors of tuberculous meningitis in adults: a 6-year retrospective study at a tertiary hospital in northern Taiwan. J Microbiol Immunol Infect. 2010 Apr;43(2):111-8. doi: 10.1016/S1684-1182(10)60018-7.
Katti MK. Immunodiagnosis of tuberculous meningitis: rapid detection of mycobacterial antigens in cerebrospinal fluid by reverse passive hemagglutination assay and their characterization by Western blotting. FEMS Immunol Med Microbiol. 2001 Jul;31(1):59-64. doi: 10.1111/j.1574-695X.2001.tb01587.x.
Luo M, Wang W, Zeng Q, Luo Y, Yang H, Yang X. Tuberculous meningitis diagnosis and treatment in adults: A series of 189 suspected cases. Exp Ther Med. 2018 Sep;16(3):2770-2776. doi: 10.3892/etm.2018.6496.
Garcia-Monco JC. Central nervous system tuberculosis. Neurol Clin. 1999 Nov;17(4):737-59. doi: 10.1016/s0733-8619(05)70164-x.
Kalita J, Misra UK. Outcome of tuberculous meningitis at 6 and 12 months: a multiple regression analysis. Int J Tuberc Lung Dis. 1999 Mar;3(3):261-5.
Hosoglu S, Geyik MF, Balik I, Aygen B, Erol S, Aygencel TG, et al. Predictors of outcome in patients with tuberculous meningitis. Int J Tuberc Lung Dis. 2002 Jan;6(1):64-70.
Misra UK, Kalita J, Roy AK, Mandal SK, Srivastava M. Role of clinical, radiological, and neurophysiological changes in predicting the outcome of tuberculous meningitis: a multivariable analysis. J Neurol Neurosurg Psychiatry. 2000 Mar;68(3):300-3. doi: 10.1136/jnnp.68.3.300.
Hsieh FY, Chia LG, Shen WC. Locations of cerebral infarctions in tuberculous meningitis. Neuroradiology. 1992;34(3):197-9. doi: 10.1007/BF00596334.
Girgis NI, Sultan Y, Farid Z, Mansour MM, Erian MW, Hanna LS, et al. Tuberculosis meningitis, Abbassia Fever Hospital-Naval Medical Research Unit No. 3-Cairo, Egypt, from 1976 to 1996. Am J Trop Med Hyg. 1998 Jan;58(1):28-34. doi: 10.4269/ajtmh.1998.58.28.
Rock RB, Hu S, Gekker G, Sheng WS, May B, Kapur V, Peterson PK. Mycobacterium tuberculosis-induced cytokine and chemokine expression by human microglia and astrocytes: effects of dexamethasone. J Infect Dis. 2005 Dec 15;192(12):2054-8. doi: 10.1086/498165.
Bidstrup C, Andersen PH, Skinhøj P, Andersen AB. Tuberculous meningitis in a country with a low incidence of tuberculosis: still a serious disease and a diagnostic challenge. Scand J Infect Dis. 2002;34(11):811-4. doi: 10.1080/0036554021000026938.
van Well GT, Paes BF, Terwee CB, Springer P, Roord JJ, Donald PR, et al. Twenty years of pediatric tuberculous meningitis: a retrospective cohort study in the western cape of South Africa. Pediatrics. 2009;123(1):e1-8. doi: 10.1542/peds.2008-1353.
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


