Classification, diagnosis of reversibility and severity assessment of patients having respiratory distress based on pulmonary function test
Abstract
Introduction: Pulmonary function testing is the gold standard for physicians to diagnose and manage respiratory problems. An obstructive defect is indicated by low forced expiratory volume in one second/forced vital capacity (FEV1/FVC) ratio, defined as less than 0.7 or below the fifth percentile. If an obstructive defect is present, the physician should determine if the disease is reversible based on the increase in FEV1 or FVC after bronchodilator treatment (i.e., increase of more than 12% and 200 ml in adults). An FVC below the fifth percentile indicates a restrictive pattern based on NHANES III data in adults. If both the FEV1/FVC ratio and the FVC are low, the patient has a mixed defect.
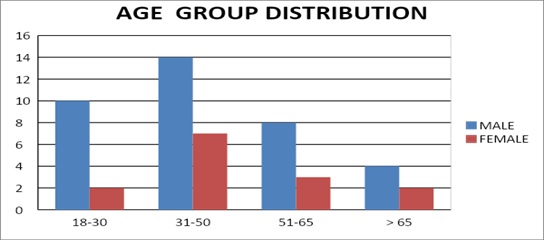
Method: A total of 60 patients having respiratory distress, who attended chest OPD underwent a pulmonary function test.
Results: In this study out of 60 patients, 32 patients had obstructive airway diseases with low FEV1/FVC (53.33%), 8 of them (13.33%) had restrictive lung diseases, ten patients(16.66%) had mixed features and rest ten patients(16.66%) had normal spirometry. Among those 32 patients of obstructive features, 22 (68.75%) had reversible airway diseases. Severity was measured among the other ten non-reversible obstructive patients according to the GOLD criteria.
Conclusion: Pulmonary function test is the fundamental first-line investigation to diagnose obstructive and restrictive lung diseases and also to differentiate between reversible and non-reversible obstruction. It is also a vital tool for determining the severity among non-reversible obstructive airway patients.
Downloads
References
Jeremy D. Johnson, MD, MPH, Tripler Army Medical Center, Honolulu, HawaiiWesley M. Theurer, do, mph, Madigan Army Medical Center, Fort Lewis, Washington Am Fam Physician. 2014;89(5):359-366.
National Asthma Education and Prevention Program. Expert Panel Report 3 (EPR-3): Guidelines for the diagnosis and management of asthma—summary report 2007. J Allergy Clin Immunol. 2007;120(5):S94-S138. doi: https://doi.org/10.1016/j.jaci.2007.09.043.
Vesbo J, Hurd SS, Agustí AG, Jones PW, Vogelmeier C, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187(4):347-365. doi: https://doi.org/10.1164/rccm.201204-0596PP.
Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi RE, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26(5):948-968. doi: https://doi.org/10.1183/09031936.05.00035205.
Standardization of spirometry, 1994 update. American Thoracic Society. Am J Respir Crit Care Med. 1995;152(3):1107-1136. doi: https://doi.org/10.1164/ajrccm.152.3.7663792.
Celli BR, Decramer M, Wedzicha JA, Wilson KC, Agustí A, Criner GJ, et al.; ATS/ERS Task Force for COPD Research. An official American Thoracic Society/European Respiratory Society statement: research questions in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2015;191(7):e2–e27. doi: https://doi.org/10.1164/rccm.201501-0044ST.
Rahmanian SD, Wood KL, Lin S, King MA, Horne A, Yang S, Wu HM, Diaz PT. Gender differences in pulmonary function, respiratory symptoms, and macrophage proteomics among HIV-infected smokers. Scientifica. 2014;2014. doi: https://doi.org/10.1155/2014/613689.
Ford ES, Mannino DM, Wheaton AG, Giles WH, Presley-Cantrell L, Croft JB. Trends in the prevalence of obstructive and restrictive lung function among adults in the United States: findings from the National Health and Nutrition Examination surveys from 1988-1994 to 2007-2010. Chest. 2013;143(5):1395-1406. doi: https://doi.org/10.1378/chest.12-1135.
Vandevoorde J, Verbanck S, Schuermans D, Kartounian J, Vincken W. Europe Resp J. 2006;27:378-383; doi: https://doi.org/10.1183/09031936.06.00036005.
Ferguson GT, Enright PL, Buist AS, Higgins MW. Office spirometry for lung health assessment in adults: a consensus statement from the National Lung Health Education Program. Chest 2000;117(4):1146-1161. doi: https://doi.org/10.1378/chest.117.4.1146.
Tashkin DP, Celli B, Decramer M, Liu D, Burkhart D, Cassino C, et al. Bronchodilator responsiveness in patients with COPD. Eur Respir J. 2008;31(4):742-750. doi: https://doi.org/10.1183/09031936.00129607.
Müller V, Gálffy G, Orosz M, Kovats Z, Odler B, Selroos O, et al. Characteristics of reversible and nonreversible COPD and asthma and COPD overlap syndrome patients: an analysis of salbutamol Easyhaler data. Int J Chron Obstruct Pulmon Dis. 2016;11:93-101. doi: https://dx.doi.org/10.2147%2FCOPD.S92331.
Postma DS, Reddel HK, ten Hacken NH, van den Berge M. Asthma and chronic obstructive pulmonary disease: similarities and differences. Clin Chest Med. 2014;35(1):143-156. doi: https://doi.org/10.1016/j.ccm.2013.09.010.
Janson C, Malinovschi A, Amaral AF, Accordini S, Bousquet J, Buist AS, et al. Bronchodilator reversibility in asthma and COPD: Findings from three large population studies, Europe Resp J. 2019;54(3):1900561. doi: https://doi.org/10.1183/13993003.00561-2019.
Barreiro TJ, Perillo I. An approach to interpreting spirometry. Am Fam Physician. 2004;69(5):1107-1114.
Aaron SD, Dales RE, Cardinal P. How accurate is spirometry at predicting restrictive pulmonary impairment? Chest. 1999;115(3):869-873. doi: https://doi.org/10.1378/chest.115.3.869.
Boros P, Franczuk M, Wesołowski S., Mixed changes in spirometry--verification of the pattern of lung function impairment; Pneumonol Alergol Pol. 2003;71(11-12):527-532.
Mapel DW, Dalal AA, Johnson P, Becker L, Hunter AG. A clinical study of COPD severity assessment by primary care physicians and their patients compared with spirometry. Am J Med. 2015;128(6):629-637. doi: https://doi.org/10.1016/j.amjmed.2014.12.018. Epub 2015 Jan 13.
Safka KA, Wald J, Wang H, McIvor L, McIvor A. GOLD Stage and Treatment in COPD: A 500 Patient Point Prevalence Study.Chronic Obstr Pulm Dis. 2017;4(1):45-55. doi: https://doi.org/10.15326/jcopdf.4.1.2016.0126.
Haughney J, Gruffydd-Jones K, Roberts J, Lee AJ, Hardwell A, McGarvey L. The distribution of COPD in UK general practice using the new GOLD classification. Europe Resp J. 2014;43(4):993-1002. doi: https://doi.org/10.1183/09031936.00065013.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


