A study of dexmedetomidine as an adjuvant to hyperbaric bupivacaine in subarachnoid block
Abstract
Background: No drug, used as adjuvant to spinal bupivacaine, has yet been identified that specifically inhibits nociception without its associated side-effects. Dexmedetomidines a novel alpha-2 agonist which holds promise as an intra-thecal adjuvant.
Aims: This observational study was conducted to evaluate the onset and duration of sensory and motor block as well as perioperative analgesia and adverse effects of dexmedetomidine given intrathecally with 0.5% hyperbaric bupivacaine for spinal anesthesia.
Materials and Methods: A total of 60 patients belonging to age group 18-60 yrs, urban population, classified as American Society of Anesthesiologists status I and II scheduled for lower abdominal and lower limb procedures were prospectively studied. Patients were randomly allocated to receive intrathecally either 12.5 mg hyperbaric bupivacaine plus 5 μg (0.5 ml) dexmedetomidine (group D, n=30) or 12.5 mg hyperbaric bupivacaine plus 0.5 ml NS (group B, n=30). Sensory and motor blockade charactersistics- The onset time to reach peak sensory and motor level, the regression time for sensory and motor block, time for rescue analgesia, hemodynamic changes and side-effects were recorded. Data collection was done by observation and measurement of various parameters.
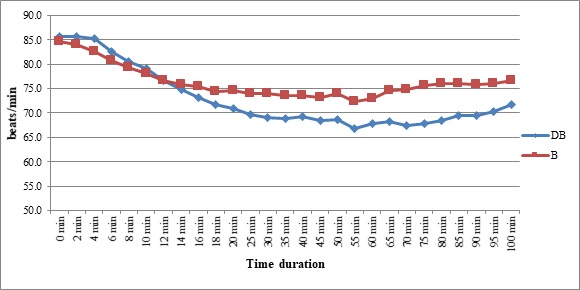
Results: The onset times to reach T10 dermatome, peak sensory level and onset time to reach modified Bromage 3 motor block were similar in both groups. We found that adding dexmedetomidine intrathecally significantly prolonged sensory and motor block time. time for first analgesic request was also significantly prolonged in group BD. Statistically there were no significant differences in hemodynamic alterations and other adverse effects between the groups.
Conclusion: clinical advantage of dexmedetomidine is that it facilitates the spread of the block and offers prolonged post‑operative analgesia. The groups were similar with respect to hemodynamic variables and there were no significant side-effects in either of the groups. However, prolonged duration of motor blockade with dexmedetomidine may be undesirable for short‑term surgical procedures or ambulatory surgeries.
Downloads
References
Liu SS. A comparison of regional versus general anesthesia for ambulatory anesthesia: a meta-analysis of randomized controlled trials. Anesth Analg2005; 101:1634-42.
McCartney CJ, Brull R, Chan VW, et al. Early but no long-term benefit of regional compared with general anesthesia for ambulatory hand surgery. Anesthesiology2004; 101:461
Kalso EA, Pöyhiä R, Rosenberg PH. Spinal antinociception by dexmedetomidine, a highly selective α2‐adrenergic agonist. Pharmacology & toxicology. 1991 Feb;68(2):140-3.
Ishii H, Kohno T, Yamakura T, Ikoma M, Baba H. Action of dexmedetomidine on the substantia gelatinosa neurons of the rat spinal cord. European Journal of Neuroscience. 2008 Jun;27(12):3182-90.
Kuzma PJ, Kline MD, Calkins MD, Staats PS. Progress in the development of ultra-long-acting local anesthetics. Reg Anesth 1997; 22:543-51.
Gulur P, Nishimori M, Ballantyne JC. Regional anaesthesia versus general anaesthesia, morbidity and mortality. Best practice & research Clinical anaesthesiology. 2006 Jun 1;20(2):249-63.
Watson B, Allen J. Spinal anaesthesia. Day Case Surgery. 2011 Nov 24:79.
Axelsson K, Gupta A. Local anaesthetic adjuvants: neuraxial versus peripheral nerve block. Current Opinion in Anesthesiology. 2009 Oct 1;22(5):649-54.
Förster JG, Rosenberg PH. Clinically useful adjuvants in regional anaesthesia. Current Opinion in Anesthesiology. 2003 Oct 1;16(5):477-86.
Davis FM, Woolner DF, Frampton C, Wilkinson A, Grant A, Harrison RT, Roberts MT, Thadaka R. Prospective, multi-centre trial of mortality following general or spinal anaesthesia for hip fracture surgery in the elderly. British journal of anaesthesia. 1987 Sep 1;59(9):1080-8.
Sunil BV, Sahana KS, Jajee PR. Dexmedetomidine as an adjuvant with hyperbaric bupivacaine for spinal anaesthesia: a double-blind controlled study. Journal of Evolution of Medical and Dental Sciences. 2013 Oct 7;2(40):7604-12.
Bajwa SJ, Kulshrestha A. Dexmedetomidine: An adjuvant making large inroads into clinical practice. Annals of medical and health sciences research. 2013;3(4):475-83.
Gupta R, Verma R, Bogra J, Kohli M, Raman R, Kushwaha JK. A comparative study of intrathecal dexmedetomidine and fentanyl as adjuvants to bupivacaine. Journal of anaesthesiology, clinical pharmacology. 2011 Jul;27(3):339.
Kanazi GE, Aouad MT, Jabbour‐Khoury SI, Al Jazzar MD, Alameddine MM, Al‐Yaman R, Bulbul M, Baraka AS. Effect of low‐dose dexmedetomidine or clonidine on the characteristics of bupivacaine spinal block. Acta AnaesthesiologicaScandinavica. 2006 Feb;50(2):222-7.
Mahendru V, Tewari A, Katyal S, Grewal A, Singh MR, Katyal R. A comparison of intrathecal dexmedetomidine, clonidine, and fentanyl as adjuvants to hyperbaric bupivacaine for lower limb surgery: A double blind controlled study. Journal of anaesthesiology, clinical pharmacology. 2013 Oct;29(4):496.
Shaikh SI, Dattatri R. Dexmedetomidine as an adjuvant to hyperbaric spinal bupivacaine for infra-umbilical procedures: A dose related study. Anaesthesia, Pain & Intensive Care. 2019 Jan 28:180-5.
Sun Y, Xu Y, Wang GN. Comparative evaluation of intrathecal bupivacaine alone, bupivacaine-fentanyl, and bupivacaine-dexmedetomidine in caesarean section. Drug research. 2015 Sep;65(09):468-7
Al-Mustafa MM, Abu-Halaweh SA, Aloweidi AS, Murshidi MM, Ammari BA, Awwad ZM, Al-Edwan GM, Ramsay MA. Effect of dexmedetomidine added to spinal bupivacaine for urological procedures. Saudi Med J. 2009 Mar 1;30(3):365-70.
Mantz J, Josserand J, Hamada S. Dexmedetomidine: new insights. European Journal of Anaesthesiology (EJA). 2011 Jan 1;28(1):3-6.
Paris A, Tonner PH. Dexmedetomidine in anaesthesia. Current Opinion in Anesthesiology. 2005 Aug 1;18(4):412-8.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


