Dosimetric parameters of heart and left ventricle – comparison of 3D CRT and IMRT in left cancer breast
Abstract
Background: Conformal Radiotherapy techniques adapting to the ballistics of delineated volumes allowed significant reduction in excess radiation induced mortality however the increasing number of long-term survivors and expanding use of cardiotoxic drug highlight the persistent need for maximal cardiac possible sparing. The low dose volume of left ventricle are better predictor of acute coronary events than mean heart dose.
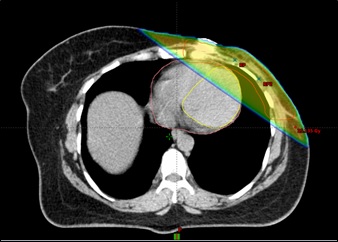
Materials and Methods: 38 post-MRM patients were randomized to treatment by 3Dimensional Conformal Radiotherapy (3D CRT) and Intensity Modulated Radiotherapy (IMRT) technique. Two tangential beams were used in 3D CRT technique while five to seven (mostly tangential beams) were used in inversely planned IMRT technique. The dose volume parameters of planning target volume, heart and left ventricle were compared.
Results: The dosimetry of Planning target volume showed significantly better coverage in IMRT technique (D90, D95) however the D50 was comparable in both the techniques. In dosimetry of heart, the high dose volumes (V30, V40) were nearly comparable in both the techniques. The other dose volume parameters (V5, V10, V20, V25, D33, D67, D100) and the mean dose were significantly lesser in 3D CRT technique along with significantly better sparing of left ventricle (Dmean and V5).
Conclusion: The dosimetry of target volume was better with IMRT technique, but this was accompanied by a huge increase in dose to whole heart and specifically the left ventricle which has strong potential to translate into an increased cardiotoxicity. A better distribution of the target region may be obtained by multiple segmentation of the two tangential fields in 3D CRT plans with further reduction in dose to heart and left ventricle.
Downloads
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6): 394-424. doi : https://doi.org/10.3322/caac.21492.
Marmot MG, Altman DG, Cameron DA, Dewar JA, Thompson SG, Wilcox M. The benefits and harms of breast cancer screening: an independent review, Br J Cancer. 2013; 108(11):2205-2240. doi: https://doi.org/10.1038/bjc.2013.177.
Kanapuru B, Ershler WB, Hesdorffer C, Jemal A, Yates JW. Long-term survival of older breast cancer patients: population-based estimates over three decades. Breast Cancer Res Treat. 2012;134(2):853-857. doi: https://doi.org/10.1007/s10549-012-2115-4.
Guarneri V, Conte PF The curability of breast cancer and the treatment of advanced disease. Eur J Nucl Med Mol Imaging. 2004; 31(1):S149-S161. doi: https://doi.org/10.1007/s00259-004-1538-5.
Shah C, Badiyan S, Berry S, Khan AJ, Goyal S, Schulte K, et al. Cardiac dose sparing and avoidance techniques in breast cancer radiotherapy. Radiotherap Oncol. 2014;112 (1): 9-16. doi: https://doi.org/10.1016/j.radonc.2014.04.009.
Lee MS, Finch W, Mahmud E. Cardiovascular complications of radiotherapy. Am J Cardiol. 2013;112 (10): 1688-1696. doi: https://doi.org/10.1016/j.amjcard.2013.07.031.
Boice Jr JD, Harvey EB, Blettner M, Stovall M, Flannery JT. Cancer in the contralateral breast after radiotherapy for breast cancer. N Engl J Med. 1992;326(12):781-785. doi: https://dx.doi.org/10.1056/NEJM199203193261201.
Bazire L, De Rycke Y, Asselain B, Fourquet A, Kirova YM. Risks of second malignancies after breast cancer treatment: Long-term results. Cancer Radiother. 2017;21 (1):10-15. doi: https://doi.org/10.1016/j.canrad.2016.07.101.
Clarke M, Collins R, Darby S Davies C, Elphinstone P, Evans V, et. al Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials Early breast cancer trialists' collaborative group (EBCTCG) The Lancet. 2006;366(9503):2087-2106. doi: https://doi.org/10.1016/S0140-6736(05)67887-7.
Gagliardi G, Constine LS, Moiseenko V, Correa C, Pierce LJ, Allen AM, et al. Radiation dose–volume effects in the heart. Int. J. Radiation Oncology Biol. Phys. 2010; 76(3):77-85. doi: https://doi.org/10.1016/j.ijrobp.2009.04.093.
van den Bogaard VA, Ta BD, van der Schaaf A, Bouma AB, Middag AM, Bantema-Joppe EJ, et al. Validation and Modification of a Prediction Model for Acute Cardiac Events in Patients with Breast Cancer Treated with Radio-therapy Based on Three-Dimensional Dose Distributions to Cardiac Substructures. J Clin Oncol. 2017; 35 (11):1171-1178. doi: https://dx.doi.org/10.1200%2FJCO.2016.69.8480.
Duane F, Aznar MC, Bartlett F, Cutter DJ, Darby SC, Jagsi R, et al. Cardiac Contouring A cardiac contouring atlas for radiotherapy. Radiother Oncol. 2017;122(3):416-422. doi: https://doi.org/10.1016/j.radonc.2017.01.008.
Vol I. Prescribing, recording, and reporting photon-beam intensity-modulated radiation therapy (IMRT): contents. J ICRU. 2010;10. doi: https://doi.org/10.1093/jicru/ndq002.
Menzel HG. International commission on radiation units and measurements. Journal of the ICRU. 2014;14 (2):1-2. doi: https://doi.org/10.1093/jicru/ndx006.
Rastogi K, Sharma S, Gupta S, Agarwal N, Bhaskar S, Jain S. Dosimetric comparison of IMRT versus 3DCRT for post-mastectomy chest wall irradiation. J Radiat Oncol. 2018; 36(1):71-78 doi: https://dx.doi.org/10.3857%2Froj.2017.00381.
Rudat V, Alaradi AA, Mohamed A, Khaled AY, Altuwaijri S. Tangential beam IMRT versus tangential beam 3D-CRT of the chest wall in postmastectomy breast cancer patients: A dosimetric comparison. Radiat Oncol J. 2011; 6(1):26. doi: https://doi.org/10.1186/1748-717X-6-26.
Kausar M, Gurjar OP, Bagdare P, Gupta KL, Bhandari V, Naik A, et al. Dosimetric analysis of intensity-modulated radiotherapy and three-dimensional conformal radiotherapy for chest wall irradiation in breast cancer patients. J Radiotherap Pract. 2016;15(1): 30-37. doi: https://doi.org/10.1017/S1460396915000503.
Aras S, İkizceli T, Aktan M. Dosimetric Comparison of Three-Dimensional Conformal Radiotherapy (3D-CRT) and Intensity Modulated Radiotherapy Techniques (IMRT) with Radiotherapy Dose Simulations for Left-Sided Mastectomy Patients; Eur J Breast Health. 2019;15(2):85-89. doi: https://dx.doi.org/10.5152%2Fejbh.2019.4619.
Finazzi T, Nguyen VT, Zimmermann F, Papachri-stofilou A. Impact of patient and treatment characteristics on heart and lung dose in adjuvant radiotherapy for left-sided breast cancer. J Rad Oncol. 2019;14(1):153. doi: https://doi.org/10.1186/s13014-019-1364-3.
Buijsen J, Jager JJ, Bovendeerd J, Voncken R, Borger JH, Boersma LJ et al. Prone breast irradiation for pendulous breasts. Radiother Oncol. 2007;82(3):337-340. doi: https://doi.org/10.1016/j.radonc.2006.08.014.
Griem KL, Fetherston P, Kuznetsova M, Foster GS, Shott S, Chu J. Three-dimensional photon dosimetry: a comparison of treatment of the intact breast in the supine and prone position. Int J Radiat Oncol Biol Phys. 2003; 57(3): 891-899. doi: https://doi.org/10.1016/S0360-3016(03)00723-5.
Varga Z, Hideghéty K, Mező T, Nikolényi A, Thurzó L, Kahán Z. Individual positioning: a comparative study of adjuvant breast radiotherapy in the prone versus supine position. Int J Radiat Oncol Biol Phys. 2009;75(1):94-100. doi: https://doi.org/10.1016/j.ijrobp.2008.10.045.
Sripathi LK, Ahlawat P, Simson DK, Khadanga CR, Kamarsu L, Surana SK, et al. Cardiac dose reduction with deep-inspiratory breath technique of radiotherapy for left-sided breast cancer. J Med Phys. 2017;42(3):123-127. doi: https://dx.doi.org/10.4103%2Fjmp.JMP_139_16.
Helal A, Elbatikhy R., Significant reductions in heart and lung doses using IMRT for left sided breast cancer patients. Pan Arab J Oncol. 2015;8(3):14-18.
Kachnic LA, Powell SN. IMRT for Breast Cancer-Balancing Outcomes, Patient Selection, and Resource Utilization, J Natl Cancer Inst.2011;103(10):777-779.doi: https://doi.org/10.1093/jnci/djr136.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


