To study the level of congestion in Pre anesthetic Check up (PAC) clinic and use of Self-answering Pre-operative questionnaire to decongest it
Abstract
Background: Aim of the study was to reduce congestion in PAC clinic, which is the direct indicator of efficiency of the hospital. 1) To study overall waiting time in the PAC clinic. 2) To suggest action to improve the waiting time in PAC.
Methods: Prospective, Descriptive study, 40 patients in each group. Group “R” = Patients registered for PAC clinic, who’s all vitals and clinical assessment was done after arrival to PAC clinic as routine practice. Group “Q” = Patients were provided Self-answering Pre-operative in waiting area and whose vital parameters were taken before arrival to PAC clinic by a trained staff. Data was recorded for both the groups.
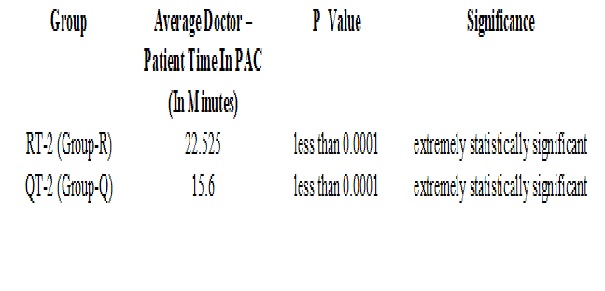
Results: We found in our study that average waiting time that is total time from registration to completion of PAC in OPD clinic was statistically significantly less in QT-1 (Group “Q”) in comparison to RT-1 (Group “R”). We found in our study that average Doctor – Patient time that is time of interaction with Doctor during PAC in OPD clinic was also statistically significantly less in QT-2 (Group “Q”) in comparison to RT-2 (Group “R”).
Conclusion: Present study was planned to reduce congestion in OPD for pre-anesthesia checkup for elective surgery or procedure. Patient satisfaction comes automatically as a byproduct with the achievement of the goal of the study. Time is money in the present scenario and thus best utilization of time with efficient outcome is the prerequisite of any good management.
Downloads
References
American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Practice advisory for preanesthesia evaluation: a report by the American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Anesthesiology. 2002 Feb; 96(2):485-96.
Klopfenstein CE, Forster A, Van Gessel E. Anesthetic assessment in an outpatient consultation clinic reduces preoperative anxiety. Can J Anaesth. 2000 Jun;47(6):511-5.DOI: https://doi.org/10.1007/BF03018941
Mendes FF, Mathias LA, Duval Neto GF, et al. Impact of preoperative outpatient evaluation clinic on performance indicators. Rev Bras Anestesiol. 2005 Apr;55(2):175-87.
Barnes PK, Emerson PA, Hajnal S et al. Influence of an anaesthetist on nurse-led, computer-based, pre-operative assessment. Anaesthesia, 2000; 55:576-580.
Organisation and Management of Hospitals, Practical Manual of PGDHHM 03. IGNOU; 2001. Patient satisfaction; pp. 14–25.
Valentine NB, Silva A, Kawabata K, et al. Health system responsiveness: concepts, domains, and operationalization. In: CJL M, Evans DB, et al., editors. Health systems performance assessment: debates, methods and empiricism. Geneva: World Health Organization; 2003. p. 96.
Silva A. A Framework for measuring responsiveness. GPE Discussion Paper Series: No. 32. EIP/GPE/EBD. Geneva: World Health Organization; 2010.
Michael M, Schaffer SD, Egan PL, et al. Improving wait times and patient satisfaction in primary care. J Healthc Qual. 2013 Mar-Apr;35(2):50-59; quiz 59-60. doi: https://doi.org/10.1111/jhq.12004.
Katre AN. Assessment of the Correlation between Appointment Scheduling and Patient Satisfaction in a Pediatric Dental Setup. Int J Dent. 2014. Article ID 453237:1–7. doi: https://doi.org/10.1155/2014/453237. [PMC free article].
Helbig M, Helbig S, Kahla-Witzsch HA, et al. Quality management: reduction of waiting time and efficiency enhancement in an ENT-university outpatients' department. BMC Health Serv Res. 2009 Jan 31;9:21. doi: https://doi.org/10.1186/1472-6963-9-21.
Pitrou I, Lecourt AC, Bailly L, et al. Waiting time and assessment of patient satisfaction in a large reference emergency department: a prospective cohort study, France. Eur J Emerg Med. 2009 Aug;16(4):177-82. doi: https://doi.org/10.1097/MEJ.0b013e32831016a6.
Anderson RT, Camacho FT, Balkrishnan R. Willing to wait?: the influence of patient wait time on satisfaction with primary care. BMC Health Serv Res. 2007 Feb 28;7:31.DOI: https://doi.org/10.1186/1472-6963-7-31.
Preyde M, Crawford K, Mullins L. et al. Patients' satisfaction and wait times at Guelph General Hospital Emergency Department before and after implementation of a process improvement project. CJEM. 2012 May;14(3):157-68.
Harper PR, Gamlin HM. Reduced outpatient waiting times with improved appointment scheduling: a simulation modeling approach. OR Spectr. 2003;25:207–222. doi: https://doi.org/10.1007/s00291-003-0122-x. [Cross Ref]
Huang XM. Patient attitude towards waiting in an outpatient clinic and its applications. Health Serv Manage Res. 1994 Feb;7(1):2-8.DOI: https://doi.org/10.1177%2F095148489400700101.
Kumari R, Idris M, Bhushan V, et al. Study on patient satisfaction in the government allopathic health facilities of lucknow district, India. Indian J Community Med. 2009 Jan;34(1):35-42. doi: https://dx.doi.org/10.4103%2F0970-0218.45372.
Harshallowalekar and N. Ravichandran. Managing the outpatient department waiting time at rajas eye hospital, IMJ, Volume 4 Issue 1 April-June, 2012; p36-46.
Mitrabasu, Predeep K Chugh, Amit Bardhan. Discrete event simulation to reduce patient waiting time in outdoor department of a tertiary care thyroid hospital, International Journal of Emerging Technology and Advanced Engineering Volume 3, Issue 9, September 2013; p.426- 431.
Pierce RA 2nd, Rogers EM, Sharp MH, et al. Outpatient pharmacy redesign to improve work flow, waiting time, and patient satisfaction. Am J Hosp Pharm. 1990 Feb;47(2):351-6.
Spaite DW, Bartholomeaux F, Guisto J, et al. Rapid process redesign in a university-based emergency department: decreasing waiting time intervals and improving patient satisfaction. Ann Emerg Med. 2002 Feb;39(2):168-77.
Adamu H, Oche MO. Patient satisfaction with services at a general outpatient clinic of a tertiary hospital in Nigeria. Br J Med Med Res. 2014;4(11):2181–2202. doi: https://doi.org/10.9734/BJMMR/2014/5918.
Hilditch WG, Asbury AJ, Jack E, et al. Validation of a pre-anaesthetic screening questionnaire. Anaesthesia. 2003 Sep;58(9):874-7.
Harding KE, Taylor NF. Highly satisfied or eager to please? Assessing satisfaction among allied health outpatients. Int J TherRehabil. 2010;17(7):353–359. doi: https://doi.org/10.12968/ijtr.2010.17.7.48892.
Anderson RT, Camacho FT, Balkrishnan R. Willing to wait?: the influence of patient wait time on satisfaction with primary care. BMC Health Serv Res. 2007 Feb 28;7:31.DOI: https://doi.org/10.1186/1472-6963-7-31.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


